Type 2 diabetes is a chronic metabolic disorder characterized by elevated blood glucose levels due to the body’s ineffective use of insulin. Unlike type 1 diabetes, which results from the pancreas not producing insulin, type 2 diabetes involves insulin resistance, where the body’s cells do not respond adequately to insulin, leading to a buildup of glucose in the bloodstream.
The prevalence of type 2 diabetes has been rising globally, posing significant health and economic challenges. It increases the risk of heart disease, stroke, kidney disease, blindness, and amputation. However, early diagnosis, lifestyle modifications, and proper management can help individuals with type 2 diabetes live long, healthy lives.
Understanding the causes, symptoms, and treatment options for type 2 diabetes is essential for effective management and prevention. This article will explore these aspects in detail, providing a comprehensive overview of this prevalent condition.
What is Type 2 Diabetes?
Type 2 diabetes is a serious and increasingly prevalent chronic condition that affects the body’s ability to regulate blood sugar levels. Understanding its key aspects is crucial for effective management and prevention.
- Chronic: Type 2 diabetes is a long-term condition that requires ongoing management.
- Metabolic: It affects the body’s metabolism, specifically the way it uses glucose for energy.
- Hyperglycemia: Elevated blood glucose levels are a hallmark characteristic of type 2 diabetes.
- Insulin Resistance: The body’s cells do not respond adequately to insulin, leading to a buildup of glucose in the bloodstream.
- Lifestyle Factors: Obesity, physical inactivity, and unhealthy diet contribute to the development of type 2 diabetes.
- Genetic Predisposition: Family history and certain genetic variations can increase the risk of developing type 2 diabetes.
- Complications: Uncontrolled type 2 diabetes can lead to severe health complications, including heart disease, stroke, kidney failure, blindness, and amputation.
These key aspects highlight the complex and multifaceted nature of type 2 diabetes. It is a chronic condition that affects the body’s metabolism, leading to elevated blood glucose levels due to insulin resistance. Understanding these aspects is essential for individuals at risk, those diagnosed with type 2 diabetes, and healthcare professionals involved in its management and prevention.
Chronic
The chronic nature of type 2 diabetes is a fundamental aspect of understanding the condition. Unlike acute illnesses that resolve within a short period, type 2 diabetes is a long-term condition that requires ongoing management throughout an individual’s life.
This chronic aspect is directly linked to the underlying pathophysiology of type 2 diabetes. The body’s inability to effectively use insulin, either due to insulin resistance or impaired insulin production, leads to persistently elevated blood glucose levels. This chronic hyperglycemia can damage various organs and tissues over time, contributing to the development of serious complications such as heart disease, stroke, kidney failure, blindness, and amputation.
Recognizing the chronic nature of type 2 diabetes is crucial for effective management. Individuals with type 2 diabetes need to adopt long-term lifestyle changes, including maintaining a healthy diet, engaging in regular physical activity, and monitoring their blood glucose levels. Medications may also be necessary to control blood sugar levels and prevent or delay complications.
Ongoing management of type 2 diabetes requires a collaborative effort between individuals, healthcare providers, and support systems. Regular medical check-ups, medication adherence, and lifestyle modifications are essential to optimize health outcomes and prevent or delay complications. By understanding the chronic nature of type 2 diabetes, individuals can take an active role in managing their condition and living long, healthy lives.
Metabolic
Type 2 diabetes is a metabolic disorder that affects the body’s ability to use glucose, the primary source of energy for the body’s cells. In type 2 diabetes, the body develops insulin resistance, a condition in which the cells do not respond properly to insulin, the hormone that allows glucose to enter the cells. As a result, glucose builds up in the bloodstream, leading to hyperglycemia, the hallmark characteristic of diabetes.
Understanding the metabolic aspect of type 2 diabetes is crucial for effective management. When the body cannot effectively use glucose for energy, it turns to alternative sources, such as breaking down fat and muscle tissue. This can lead to weight loss, fatigue, and other complications. Additionally, chronic hyperglycemia can damage the blood vessels and nerves, contributing to the development of serious complications such as heart disease, stroke, kidney failure, blindness, and amputation.
By understanding the metabolic connection in type 2 diabetes, healthcare providers and individuals can develop effective management strategies. This includes lifestyle modifications such as following a healthy diet, engaging in regular physical activity, and maintaining a healthy weight. Medications may also be necessary to improve insulin sensitivity and control blood glucose levels. Regular monitoring of blood glucose levels and HbA1c, a measure of long-term blood glucose control, is essential to assess the effectiveness of management strategies and make necessary adjustments.
Hyperglycemia
Hyperglycemia, or elevated blood glucose levels, is a defining characteristic of type 2 diabetes. It occurs when the body cannot effectively use insulin, a hormone that allows glucose to enter cells for energy production. This leads to a buildup of glucose in the bloodstream, resulting in hyperglycemia.
Understanding hyperglycemia is crucial for comprehending the pathophysiology, complications, and management of type 2 diabetes. Chronic hyperglycemia can damage blood vessels and nerves, contributing to the development of serious health complications such as heart disease, stroke, kidney failure, blindness, and amputation. Therefore, controlling blood glucose levels is a primary goal in the management of type 2 diabetes to prevent or delay these complications.
Regular monitoring of blood glucose levels through self-monitoring devices or HbA1c testing is essential for assessing the effectiveness of diabetes management strategies. Lifestyle modifications, including a healthy diet, regular physical activity, and weight management, play a vital role in controlling blood glucose levels. Medications may also be necessary to improve insulin sensitivity and lower blood glucose levels.
In summary, hyperglycemia is a hallmark characteristic of type 2 diabetes and a major contributor to its associated complications. Understanding the connection between hyperglycemia and type 2 diabetes is essential for effective management and prevention of complications.
Insulin Resistance
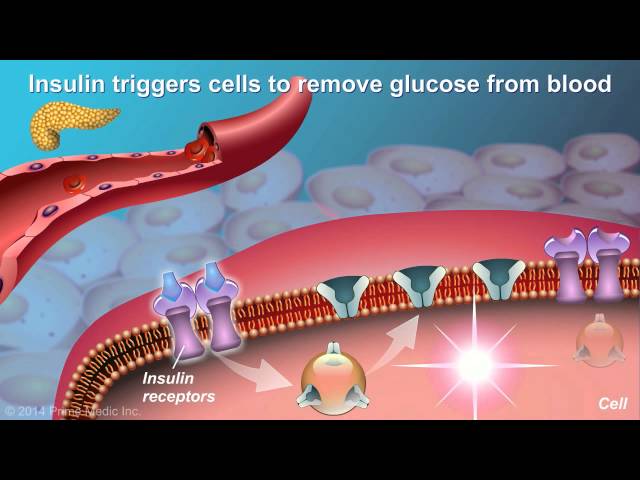
Insulin resistance is a central component of type 2 diabetes, playing a pivotal role in its development and progression. Insulin, a hormone produced by the pancreas, allows glucose to enter cells for energy production. In type 2 diabetes, the body’s cells become resistant to insulin, impairing glucose uptake and leading to a buildup of glucose in the bloodstream, a condition known as hyperglycemia.
The exact cause of insulin resistance is not fully understood, but several factors are believed to contribute, including obesity, physical inactivity, and genetics. Obesity, especially around the abdomen, is strongly linked to insulin resistance. Excess body fat releases hormones and inflammatory factors that can interfere with insulin signaling and promote insulin resistance.
Physical inactivity is another significant contributor to insulin resistance. Regular exercise improves insulin sensitivity, allowing cells to better utilize glucose. Conversely, a sedentary lifestyle can lead to insulin resistance and an increased risk of type 2 diabetes.
Insulin resistance has significant implications for overall health. It is not only a hallmark of type 2 diabetes but also a precursor to the development of other metabolic disorders, such as cardiovascular disease, fatty liver disease, and certain types of cancer.
Understanding the connection between insulin resistance and type 2 diabetes is crucial for effective management and prevention. Lifestyle modifications, including weight loss, regular exercise, and a healthy diet, can improve insulin sensitivity and reduce the risk of developing type 2 diabetes. Early detection and intervention are key to preventing or delaying the onset of type 2 diabetes and its associated complications.
Lifestyle Factors
Lifestyle factors play a significant role in the development of type 2 diabetes. Obesity, physical inactivity, and an unhealthy diet are major contributing factors to this chronic condition.
Obesity, particularly abdominal obesity, is strongly linked to insulin resistance, a key characteristic of type 2 diabetes. Excess body fat releases hormones and inflammatory factors that interfere with insulin signaling, impairing glucose uptake by cells. This leads to a buildup of glucose in the bloodstream, eventually contributing to the development of type 2 diabetes.
Physical inactivity is another important lifestyle factor that contributes to insulin resistance and type 2 diabetes risk. Regular exercise improves insulin sensitivity, allowing cells to better utilize glucose. Conversely, a sedentary lifestyle promotes insulin resistance and increases the likelihood of developing type 2 diabetes.
Unhealthy diet, characterized by excessive intake of processed foods, sugary drinks, and unhealthy fats, also plays a significant role in the development of type 2 diabetes. These foods can lead to weight gain, insulin resistance, and impaired glucose metabolism, all of which contribute to the development of type 2 diabetes.
Understanding the connection between lifestyle factors and type 2 diabetes is crucial for effective prevention and management. By maintaining a healthy weight, engaging in regular physical activity, and adopting a balanced diet, individuals can reduce their risk of developing type 2 diabetes and its associated complications.
Genetic Predisposition
Genetic predisposition plays a significant role in the development of type 2 diabetes. Family history and certain genetic variations can increase an individual’s risk of developing this chronic condition.
- Family History: Having a family history of type 2 diabetes is a significant risk factor. Studies have shown that individuals with a parent or sibling with type 2 diabetes are more likely to develop the condition themselves.
- Genetic Variations: Researchers have identified specific genetic variations that are associated with an increased risk of type 2 diabetes. These variations can affect genes involved in insulin production, insulin signaling, and glucose metabolism.
- Interaction of Genes and Environment: While genetics play a role in type 2 diabetes, it is important to note that environmental factors also interact with genetic predisposition. Factors such as obesity, physical inactivity, and unhealthy diet can increase the risk of developing type 2 diabetes, even in individuals with a genetic predisposition.
- Precision Medicine: Understanding the genetic basis of type 2 diabetes has led to the development of personalized medicine approaches. By identifying individuals at high risk based on their genetic profile, healthcare providers can implement targeted prevention and treatment strategies.
The connection between genetic predisposition and type 2 diabetes highlights the complex interplay between genetics and lifestyle factors in the development of this condition. By understanding the genetic risk factors and adopting a healthy lifestyle, individuals can reduce their risk of developing type 2 diabetes and improve their overall health and well-being.
Complications
Uncontrolled type 2 diabetes can lead to various severe health complications, including heart disease, stroke, kidney failure, blindness, and amputation. These complications are directly linked to the chronic hyperglycemia and metabolic disturbances associated with type 2 diabetes.
Chronic hyperglycemia damages blood vessels and nerves throughout the body. This damage can lead to atherosclerosis, a condition characterized by the buildup of plaque in the arteries. Atherosclerosis increases the risk of heart attack and stroke. Additionally, high blood glucose levels can weaken the heart muscle, leading to heart failure.
Diabetes-related kidney disease is another common complication of uncontrolled type 2 diabetes. Chronic hyperglycemia can damage the delicate filtering units in the kidneys, leading to a decline in kidney function. If left untreated, kidney disease can progress to kidney failure, requiring dialysis or kidney transplantation.
Diabetic retinopathy is a complication of type 2 diabetes that affects the eyes. Chronic hyperglycemia can damage the blood vessels in the retina, leading to vision problems and even blindness. Diabetic neuropathy is another common complication, characterized by nerve damage that can cause pain, numbness, and tingling in the hands, feet, and legs.
Understanding the potential complications of uncontrolled type 2 diabetes is crucial for effective management and prevention. Maintaining good blood glucose control through lifestyle modifications, medication, and regular monitoring can significantly reduce the risk of developing these complications. Early detection and intervention are key to preserving health and well-being in individuals with type 2 diabetes.
Frequently Asked Questions about Type 2 Diabetes
This section addresses common concerns and misconceptions about type 2 diabetes, providing concise and informative answers to frequently asked questions.
Question 1: What is type 2 diabetes?
Type 2 diabetes is a chronic metabolic disorder characterized by elevated blood glucose levels due to the body’s ineffective use of insulin. Insulin is a hormone that allows glucose to enter cells for energy production.
Question 2: What causes type 2 diabetes?
Type 2 diabetes is primarily caused by a combination of genetic predisposition and lifestyle factors. Obesity, physical inactivity, and unhealthy diet increase the risk of developing type 2 diabetes.
Question 3: What are the symptoms of type 2 diabetes?
Common symptoms of type 2 diabetes include frequent urination, excessive thirst, unexplained weight loss, increased hunger, fatigue, and blurred vision.
Question 4: How is type 2 diabetes diagnosed?
Type 2 diabetes is diagnosed through blood tests that measure blood glucose levels. These tests include the fasting plasma glucose test, oral glucose tolerance test, and HbA1c test.
Question 5: How is type 2 diabetes treated?
Treatment for type 2 diabetes typically involves lifestyle modifications, such as maintaining a healthy weight, engaging in regular physical activity, and following a balanced diet. Medications may also be prescribed to lower blood glucose levels.
Question 6: Can type 2 diabetes be prevented?
While type 2 diabetes cannot be completely prevented, the risk of developing it can be reduced by adopting a healthy lifestyle, including maintaining a healthy weight, engaging in regular physical activity, and following a balanced diet.
Understanding these key questions and answers about type 2 diabetes can help individuals make informed decisions about their health and well-being.
Transition to the next article section: Managing Type 2 Diabetes: A Comprehensive Guide
Tips for Managing Type 2 Diabetes
Effectively managing type 2 diabetes requires a multifaceted approach that includes lifestyle modifications, medication adherence, and regular monitoring. Here are some essential tips to help individuals manage their condition effectively:
Tip 1: Maintain a Healthy Weight
Excess weight, particularly around the abdomen, contributes to insulin resistance. Losing even a small amount of weight can significantly improve blood glucose control. Set realistic weight loss goals and make gradual changes to your diet and exercise routine.
Tip 2: Engage in Regular Physical Activity
Exercise improves insulin sensitivity and helps control blood glucose levels. Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week. Choose activities you enjoy and incorporate them into your daily routine.
Tip 3: Follow a Healthy Diet
A balanced diet is crucial for managing type 2 diabetes. Focus on consuming whole, unprocessed foods such as fruits, vegetables, lean protein, and whole grains. Limit your intake of sugary drinks, processed foods, and unhealthy fats.
Tip 4: Take Medications as Prescribed
Medications play a vital role in controlling blood glucose levels in type 2 diabetes. Take your medications exactly as prescribed by your healthcare provider and do not skip or stop taking them without consulting them first.
Tip 5: Monitor Your Blood Glucose Levels Regularly
Regular blood glucose monitoring is essential for assessing your diabetes management plan’s effectiveness. Use a blood glucose meter to check your blood glucose levels as directed by your healthcare provider.
Tip 6: Quit Smoking
Smoking worsens insulin resistance and increases the risk of diabetes complications. Quitting smoking is one of the most significant steps you can take to improve your overall health and diabetes management.
Tip 7: Manage Stress
Chronic stress can elevate blood glucose levels. Engage in stress-reducing activities such as exercise, yoga, meditation, or spending time in nature.
Tip 8: Get Enough Sleep
Lack of sleep can disrupt hormone levels and impair insulin sensitivity. Aim for 7-8 hours of quality sleep each night to support your diabetes management efforts.
Summary: By following these tips, individuals with type 2 diabetes can effectively manage their condition, improve their overall health, and reduce the risk of complications. Remember to consult with your healthcare provider regularly to tailor these recommendations to your specific needs and circumstances.
Transition to the article’s conclusion: The Road to Successful Type 2 Diabetes Management
Conclusion
Type 2 diabetes is a serious metabolic disorder characterized by elevated blood glucose levels due to insulin resistance. It is a prevalent condition with significant health implications, increasing the risk of heart disease, stroke, kidney disease, blindness, and amputation.
This article comprehensively explored the key aspects of type 2 diabetes, from its causes and symptoms to its complications and management strategies. Understanding these aspects is crucial for individuals at risk, those diagnosed with type 2 diabetes, and healthcare professionals involved in its management and prevention.
Effective management of type 2 diabetes requires a multifaceted approach that includes lifestyle modifications, medication adherence, and regular monitoring. By maintaining a healthy weight, engaging in regular physical activity, following a balanced diet, and taking medications as prescribed, individuals with type 2 diabetes can improve their blood glucose control, reduce the risk of complications, and live long, healthy lives.
Ongoing research and advancements in diabetes care continue to provide new insights and treatment options. The future of type 2 diabetes management holds promise for improved outcomes and a better quality of life for those affected by this condition.
Youtube Video: