What is type 2 diabetes mellitus? Type 2 diabetes mellitus is a chronic metabolic disorder characterized by elevated blood glucose levels due to insulin resistance and relative insulin deficiency. Insulin is a hormone produced by the pancreas that allows glucose to enter cells for energy production.
In type 2 diabetes, the body’s cells become less responsive to insulin, leading to a buildup of glucose in the bloodstream. Over time, high blood glucose levels can damage blood vessels and organs, increasing the risk of heart disease, stroke, kidney disease, and blindness.
Type 2 diabetes is the most common form of diabetes, accounting for about 90-95% of all cases. It typically develops in adulthood, although it can occur in children and adolescents. Risk factors for type 2 diabetes include obesity, physical inactivity, family history of diabetes, and certain ethnicities.
Treatment for type 2 diabetes typically involves lifestyle changes, such as weight loss, regular exercise, and a healthy diet. Medications may also be prescribed to help lower blood glucose levels.
What is type 2 diabetes mellitus?
Type 2 diabetes mellitus is a chronic metabolic disorder characterized by elevated blood glucose levels due to insulin resistance and relative insulin deficiency.
- Chronic: Type 2 diabetes is a lifelong condition that requires ongoing management.
- Metabolic: Diabetes affects the way the body converts food into energy.
- Elevated blood glucose: High blood sugar levels are a hallmark of diabetes.
- Insulin resistance: The body’s cells do not respond properly to insulin.
- Relative insulin deficiency: The pancreas does not produce enough insulin to overcome insulin resistance.
- Type 2: This is the most common type of diabetes, accounting for about 90-95% of all cases.
These key aspects highlight the important characteristics of type 2 diabetes mellitus. Understanding these aspects is crucial for effective management and prevention of the condition.
Chronic
Thenature of type 2 diabetes mellitus is a key aspect that sets it apart from other conditions. It means that once a person develops type 2 diabetes, they will need to manage it for the rest of their life. There is currently no cure for type 2 diabetes, but it can be managed with lifestyle changes and medication.
- Requires ongoing management: People with type 2 diabetes need to monitor their blood sugar levels regularly, make healthy lifestyle choices, and take medication as prescribed. This ongoing management is essential to prevent complications and maintain a good quality of life.
- Lifestyle changes: Healthy lifestyle changes, such as losing weight, eating a healthy diet, and getting regular exercise, can help to improve blood sugar control and reduce the risk of complications.
- Medication: People with type 2 diabetes may need to take medication to help lower their blood sugar levels. There are different types of diabetes medications available, and the best type of medication for each person will vary depending on their individual needs.
The chronic nature of type 2 diabetes mellitus means that it is a condition that requires ongoing care and management. However, with proper management, people with type 2 diabetes can live long, healthy lives.
Metabolic
Type 2 diabetes mellitus is a metabolic disorder, meaning that it affects the way the body converts food into energy. Insulin is a hormone that helps glucose, or sugar, from the blood enter cells for energy production. In people with type 2 diabetes, the body’s cells become resistant to insulin, and the pancreas does not produce enough insulin to overcome this resistance. As a result, glucose builds up in the bloodstream.
- Glucose metabolism: Glucose is the body’s main source of energy. In people with type 2 diabetes, the body is unable to effectively use glucose for energy, leading to high blood sugar levels.
- Insulin resistance: Insulin resistance is a key factor in the development of type 2 diabetes. When the body’s cells become resistant to insulin, they do not respond to the hormone’s signal to take in glucose from the bloodstream.
- Pancreatic beta-cell function: The pancreas produces insulin in beta cells. In type 2 diabetes, the beta cells may not produce enough insulin to overcome insulin resistance, leading to high blood sugar levels.
- Other metabolic pathways: Diabetes can also affect other metabolic pathways, such as fat and protein metabolism. This can lead to weight loss, increased thirst, and fatigue.
The metabolic effects of type 2 diabetes can have a significant impact on a person’s health and well-being. By understanding these effects, healthcare professionals can develop more effective strategies for managing and preventing type 2 diabetes.
Elevated blood glucose
Elevated blood glucose, or high blood sugar, is a defining characteristic of diabetes, including type 2 diabetes mellitus. It results from the body’s inability to effectively use glucose for energy, leading to its accumulation in the bloodstream. Understanding the connection between elevated blood glucose and type 2 diabetes is crucial for effective management and prevention.
- Insulin Resistance and Pancreatic Function: In type 2 diabetes, the body’s cells become resistant to insulin, a hormone that allows glucose to enter cells. Additionally, the pancreas may not produce enough insulin to overcome this resistance. Consequently, glucose remains in the bloodstream, leading to elevated blood glucose levels.
- Symptoms and Complications: High blood sugar levels can cause various symptoms, including increased thirst, frequent urination, fatigue, and blurred vision. Over time, sustained elevated blood glucose can damage blood vessels and organs, increasing the risk of heart disease, stroke, kidney disease, and blindness.
- Monitoring and Management: Regular monitoring of blood glucose levels is essential for managing type 2 diabetes. This monitoring allows individuals to adjust their lifestyle, medication, or insulin dosage as needed to maintain optimal blood sugar control and prevent complications.
- Lifestyle Modifications: Adopting a healthy lifestyle, including regular exercise, a balanced diet, and maintaining a healthy weight, can help improve insulin sensitivity and lower blood glucose levels. These modifications can reduce the risk of developing or worsening type 2 diabetes.
In conclusion, elevated blood glucose is a central feature of type 2 diabetes mellitus, resulting from insulin resistance and pancreatic dysfunction. It is associated with various symptoms and long-term complications. Effective management of type 2 diabetes involves regular monitoring, lifestyle modifications, and medical interventions to maintain optimal blood glucose levels and prevent associated health risks.
Insulin resistance
Insulin resistance is a condition in which the body’s cells do not respond properly to insulin, a hormone that helps glucose from the blood enter cells for energy production. This can lead to high blood sugar levels, which can cause type 2 diabetes and other health problems.
- Causes of insulin resistance: Insulin resistance can be caused by a number of factors, including obesity, physical inactivity, and family history of diabetes.
- Symptoms of insulin resistance: Insulin resistance often does not cause any symptoms, but it can lead to high blood sugar levels, which can cause symptoms such as increased thirst, frequent urination, fatigue, and blurred vision.
- Complications of insulin resistance: Insulin resistance can lead to a number of complications, including type 2 diabetes, heart disease, stroke, kidney disease, and blindness.
- Treatment for insulin resistance: There is no cure for insulin resistance, but it can be managed with lifestyle changes, such as losing weight, eating a healthy diet, and getting regular exercise. Medication may also be prescribed to help lower blood sugar levels.
Insulin resistance is a serious condition that can lead to a number of health problems. However, it can be managed with lifestyle changes and medication. If you are at risk for insulin resistance, talk to your doctor about ways to prevent or manage the condition.
Relative insulin deficiency
In the context of type 2 diabetes mellitus, relative insulin deficiency plays a crucial role in the development and progression of the condition. Insulin resistance, as discussed earlier, refers to the reduced responsiveness of body cells to insulin, impairing glucose uptake and utilization. Relative insulin deficiency compounds this issue, further exacerbating the metabolic disturbances characteristic of type 2 diabetes mellitus.
- Impaired Insulin Secretion: In type 2 diabetes, the pancreas, responsible for insulin production, may not secrete sufficient insulin to compensate for the prevailing insulin resistance. This relative deficiency arises from the failure of beta cells within the pancreas to produce and release adequate amounts of insulin.
- Progressive Beta-Cell Dysfunction: Over time, the beta cells in the pancreas may undergo progressive dysfunction, leading to a further decline in insulin production. This deterioration contributes to the worsening of insulin deficiency and the perpetuation of hyperglycemia in type 2 diabetes mellitus.
- Role in Hyperglycemia: The relative insulin deficiency, coupled with insulin resistance, results in an inability of the body to effectively regulate blood glucose levels. Glucose accumulates in the bloodstream, leading to the characteristic hyperglycemia associated with type 2 diabetes mellitus.
- Long-Term Complications: Sustained hyperglycemia due to relative insulin deficiency can lead to various long-term complications, including damage to blood vessels, nerves, and organs. These complications can manifest as cardiovascular disease, diabetic neuropathy, retinopathy, and nephropathy.
In summary, relative insulin deficiency, characterized by the pancreas’s inability to produce enough insulin to overcome insulin resistance, is a critical factor in the development and progression of type 2 diabetes mellitus. It contributes to hyperglycemia and the associated long-term complications, underscoring the importance of managing both insulin resistance and insulin deficiency in the treatment of type 2 diabetes mellitus.
Type 2
Understanding the prevalence of Type 2 diabetes as the most common type, accounting for approximately 90-95% of all diabetes cases, is a crucial aspect of defining “what type 2 diabetes mellitus is.” This high prevalence underscores the significance of Type 2 diabetes as a global health concern, impacting a vast majority of individuals with diabetes.
The widespread occurrence of Type 2 diabetes highlights the urgent need for effective prevention and management strategies. Public health initiatives aimed at promoting healthy lifestyles, raising awareness about diabetes risk factors, and facilitating early detection are essential in combating the growing prevalence of Type 2 diabetes.
Furthermore, the high prevalence of Type 2 diabetes emphasizes the importance of research efforts dedicated to understanding its underlying mechanisms, developing novel therapies, and improving patient outcomes. By unraveling the complexities of Type 2 diabetes, we can pave the way for more personalized and effective approaches to diabetes care.
In summary, the prevalence of Type 2 diabetes as the most common type of diabetes underscores its significance as a global health concern and emphasizes the need for comprehensive efforts in prevention, management, and research to address this prevalent condition effectively.
FAQs about Type 2 Diabetes Mellitus
This section addresses frequently asked questions to provide a comprehensive understanding of Type 2 diabetes mellitus.
Question 1: What is Type 2 diabetes mellitus?
Answer: Type 2 diabetes mellitus is a chronic metabolic disorder characterized by elevated blood glucose levels due to insulin resistance and relative insulin deficiency.
Question 2: What are the symptoms of Type 2 diabetes mellitus?
Answer: Common symptoms include increased thirst, frequent urination, unexplained weight loss, fatigue, and blurred vision.
Question 3: What causes Type 2 diabetes mellitus?
Answer: The exact cause is unknown, but risk factors include obesity, physical inactivity, family history, and certain ethnicities.
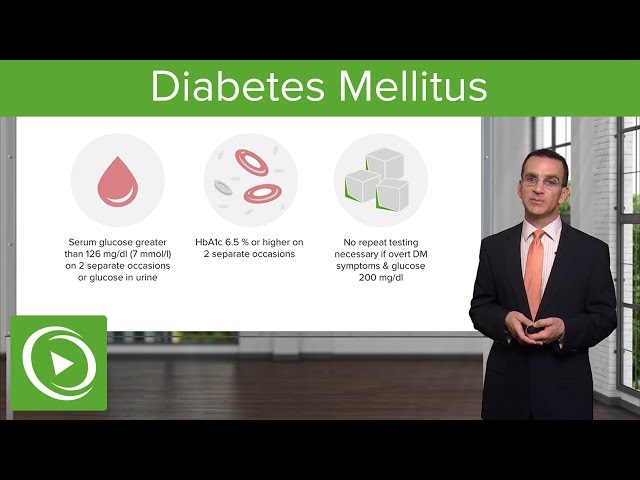
Question 4: How is Type 2 diabetes mellitus diagnosed?
Answer: Diagnosis is typically made through blood tests, such as fasting plasma glucose or oral glucose tolerance test.
Question 5: How is Type 2 diabetes mellitus treated?
Answer: Treatment involves lifestyle modifications (e.g., weight loss, exercise, healthy diet) and medications to lower blood glucose levels.
Question 6: What are the complications of Type 2 diabetes mellitus?
Answer: Untreated or poorly controlled diabetes can lead to serious complications such as heart disease, stroke, kidney disease, and blindness.
Summary: Type 2 diabetes mellitus is a common chronic condition that requires ongoing management to prevent complications. Understanding the condition and its management is crucial for maintaining good health and well-being.
Transition to the next article section: For more in-depth information about Type 2 diabetes mellitus, please refer to the next section of this article.
Tips to Manage Type 2 Diabetes Mellitus
Effectively managing Type 2 Diabetes Mellitus requires adopting healthy lifestyle practices and adhering to prescribed medical advice. Here are some essential tips to help individuals manage their condition:
Tip 1: Maintain a Healthy Diet: Prioritize a balanced diet rich in fruits, vegetables, whole grains, and lean protein. Limit processed foods, sugary drinks, and unhealthy fats to regulate blood glucose levels.
Tip 2: Engage in Regular Exercise: Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week. Exercise improves insulin sensitivity and blood sugar control.
Tip 3: Monitor Blood Glucose Levels: Regularly check blood glucose levels as recommended by your healthcare provider. This monitoring helps track progress, adjust medications, and prevent complications.
Tip 4: Take Medications as Prescribed: If medications are prescribed, adhere to the prescribed dosage and schedule. Medications can help lower blood glucose levels and manage symptoms.
Tip 5: Quit Smoking: Smoking damages blood vessels and worsens diabetes complications. Quitting smoking significantly improves overall health and diabetes management.
Tip 6: Manage Stress: Chronic stress can elevate blood glucose levels. Engage in stress-reducing activities such as yoga, meditation, or spending time in nature.
Tip 7: Get Enough Sleep: Sleep deprivation can impair insulin sensitivity. Aim for 7-9 hours of quality sleep each night to regulate blood sugar levels.
Tip 8: See Your Doctor Regularly: Schedule regular check-ups with your healthcare provider to monitor progress, adjust treatment plans, and prevent complications.
Summary: By following these tips, individuals with Type 2 Diabetes Mellitus can effectively manage their condition, improve their overall health, and reduce the risk of complications.
Transition to the article’s conclusion: Managing Type 2 Diabetes Mellitus is an ongoing journey that requires commitment and collaboration between individuals and their healthcare team. By adopting these essential tips, individuals can take control of their health and live fulfilling lives.
Conclusion
Type 2 diabetes mellitus is a complex metabolic disorder that requires ongoing management and lifestyle modifications. This article has explored the various aspects of type 2 diabetes mellitus, including its definition, causes, symptoms, diagnosis, treatment, and management tips.
Understanding the nature of type 2 diabetes mellitus is crucial for effective prevention and management. By adopting healthy lifestyle practices, adhering to prescribed medical advice, and working closely with healthcare professionals, individuals can effectively manage their condition and improve their quality of life. Ongoing research and advancements in diabetes care provide hope for even more effective treatments and improved outcomes in the future.
Youtube Video: