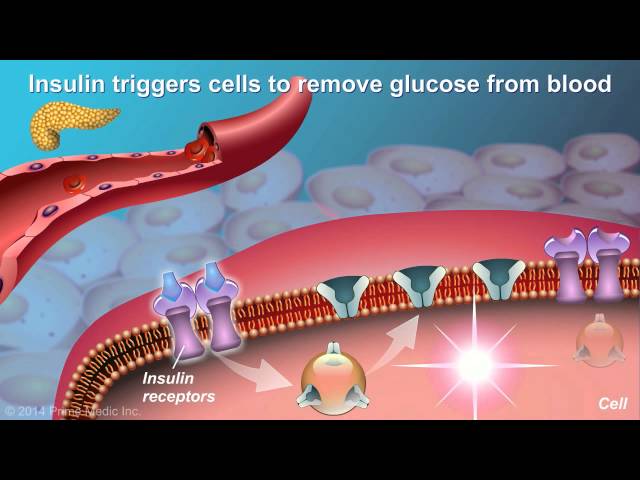
Type 2 diabetes is a chronic condition that affects the way your body uses sugar (glucose). With type 2 diabetes, your body doesn’t make enough insulin or doesn’t use insulin well. Glucose then can’t get into your cells for use as energy. Over time, high blood sugar levels can damage your heart, blood vessels, eyes, kidneys, and nerves.
There are many risk factors for type 2 diabetes, including:
- Obesity
- Physical inactivity
- Family history of diabetes
- Age (over 45)
- Race/ethnicity (African Americans, Hispanic Americans, American Indians, and Asian Americans are at increased risk)
- Certain medical conditions, such as Polycystic Ovary Syndrome (PCOS) or Gestational Diabetes
If you have any of these risk factors, it’s important to talk to your doctor about ways to reduce your risk of developing type 2 diabetes.
What Causes Type 2 Diabetes
Type 2 diabetes is a chronic condition that affects the way your body uses sugar (glucose). There are many risk factors for type 2 diabetes, including obesity, physical inactivity, family history of diabetes, age (over 45), race/ethnicity, and certain medical conditions.
- Obesity: Obesity is a major risk factor for type 2 diabetes. People who are obese are more likely to have insulin resistance, which is a condition in which the body does not use insulin well. Insulin resistance can lead to high blood sugar levels, which over time can damage the blood vessels and organs.
- Physical inactivity: Physical activity helps to improve insulin sensitivity and lower blood sugar levels. People who are physically inactive are more likely to develop type 2 diabetes.
- Family history of diabetes: People who have a family history of diabetes are more likely to develop the condition themselves. This is because genes play a role in the development of type 2 diabetes.
- Age (over 45): The risk of developing type 2 diabetes increases with age. This is because as we age, our bodies become less able to use insulin effectively.
- Race/ethnicity: African Americans, Hispanic Americans, American Indians, and Asian Americans are at increased risk for type 2 diabetes. This is due to a combination of genetic and environmental factors.
- Certain medical conditions: Certain medical conditions, such as Polycystic Ovary Syndrome (PCOS) or Gestational Diabetes, can increase the risk of developing type 2 diabetes.
These are just some of the key risk factors for type 2 diabetes. If you have any of these risk factors, it is important to talk to your doctor about ways to reduce your risk of developing the condition.
Obesity
Obesity is a major risk factor for type 2 diabetes because it can lead to insulin resistance. Insulin resistance occurs when the body’s cells do not respond well to insulin, a hormone that helps glucose enter cells for energy. When cells are resistant to insulin, glucose builds up in the blood, leading to high blood sugar levels. Over time, high blood sugar levels can damage the blood vessels and organs, leading to complications such as heart disease, stroke, kidney disease, and blindness.
- Adipose tissue dysfunction: Obesity is associated with increased adipose tissue (body fat), which can lead to inflammation and the release of hormones that interfere with insulin signaling.
- Ectopic fat accumulation: In obesity, fat can accumulate in non-adipose tissues, such as the liver and muscle, which can impair insulin sensitivity in these tissues.
- Metabolic dysregulation: Obesity can disrupt metabolism, leading to alterations in glucose and lipid metabolism that contribute to insulin resistance.
- Genetic factors: Obesity and insulin resistance share a genetic basis, with certain gene variants increasing susceptibility to both conditions.
These factors collectively contribute to the development of insulin resistance and type 2 diabetes in obese individuals. By understanding the mechanisms linking obesity to type 2 diabetes, we can develop more effective strategies for preventing and treating these conditions.
Physical inactivity
Physical inactivity is a major risk factor for type 2 diabetes. When you are physically active, your muscles use glucose for energy. This helps to lower blood sugar levels. Exercise also helps to improve insulin sensitivity, which means that your cells are better able to use insulin to take glucose from the blood. People who are physically inactive are more likely to have insulin resistance, which can lead to high blood sugar levels and type 2 diabetes.
- Facet 1: Reduced glucose uptake by muscles: Physical activity stimulates glucose uptake by muscles, which helps to lower blood sugar levels. In contrast, physical inactivity leads to decreased glucose uptake by muscles, contributing to elevated blood sugar levels.
- Facet 2: Impaired insulin signaling: Exercise enhances insulin sensitivity by improving insulin signaling pathways. Physical inactivity, on the other hand, can impair insulin signaling, making cells less responsive to insulin and reducing glucose uptake.
- Facet 3: Increased inflammation: Physical inactivity is associated with chronic low-grade inflammation, which can interfere with insulin signaling and promote insulin resistance. Regular exercise has anti-inflammatory effects, helping to mitigate inflammation and improve insulin sensitivity.
- Facet 4: Dysregulation of metabolism: Physical inactivity disrupts metabolic processes, including glucose and lipid metabolism. This can lead to an accumulation of glucose in the blood and contribute to insulin resistance.
Overall, physical inactivity contributes to the development of type 2 diabetes by reducing glucose uptake by muscles, impairing insulin signaling, increasing inflammation, and disrupting metabolism. Regular physical activity, on the other hand, helps to improve insulin sensitivity, lower blood sugar levels, and reduce the risk of type 2 diabetes.
Family history of diabetes
A family history of diabetes is a significant risk factor for developing type 2 diabetes. This is because genes play a role in the development of the condition. Studies have shown that people with a family history of diabetes are more likely to have insulin resistance, which is a condition in which the body does not use insulin well. Insulin resistance can lead to high blood sugar levels, which over time can damage the blood vessels and organs.
There are a number of genes that have been linked to type 2 diabetes. These genes are involved in various aspects of glucose metabolism, including insulin production, insulin signaling, and glucose transport. Mutations in these genes can lead to impaired glucose metabolism and an increased risk of developing type 2 diabetes.
While genetics play a role in the development of type 2 diabetes, it is important to note that it is not the only factor. Lifestyle factors, such as obesity and physical inactivity, also play a significant role. People who have a family history of diabetes can reduce their risk of developing the condition by maintaining a healthy weight, getting regular exercise, and eating a healthy diet.
If you have a family history of diabetes, it is important to talk to your doctor about ways to reduce your risk of developing the condition. Your doctor may recommend lifestyle changes, such as losing weight or getting more exercise. They may also recommend screening for diabetes so that it can be diagnosed and treated early.
Age (over 45)
As we age, our bodies undergo several changes that can affect our risk of developing type 2 diabetes. One of the most significant changes is a decline in insulin sensitivity. Insulin is a hormone that helps glucose enter cells for energy. When we are young, our bodies are able to produce enough insulin and use it effectively to keep our blood sugar levels in a healthy range.
- Facet 1: Reduced beta-cell function: With age, the pancreas produces less insulin. This is because the beta cells, which are responsible for producing insulin, gradually decline in number and function.
- Facet 2: Impaired insulin signaling: As we age, our cells become less responsive to insulin. This means that even if the pancreas is producing enough insulin, the cells may not be able to use it effectively to take glucose from the blood.
- Facet 3: Increased inflammation: Chronic inflammation is associated with aging and can contribute to insulin resistance. Inflammation can damage cells and interfere with insulin signaling.
- Facet 4: Changes in body composition: As we age, we tend to lose muscle mass and gain weight. This can lead to increased insulin resistance, as muscle is a major site of glucose uptake.
These age-related changes can lead to insulin resistance and high blood sugar levels, which over time can increase the risk of developing type 2 diabetes. It is important for older adults to be aware of these risks and to take steps to maintain a healthy weight, get regular exercise, and eat a healthy diet.
Race/ethnicity
Certain racial and ethnic groups are at increased risk for developing type 2 diabetes. This is due to a combination of genetic, socioeconomic, and cultural factors.
- Genetic factors: Certain genetic variants are more common in certain racial and ethnic groups, and these variants can increase the risk of developing type 2 diabetes. For example, African Americans have a higher prevalence of a variant in the KCNJ11 gene, which has been linked to an increased risk of type 2 diabetes.
- Socioeconomic factors: Racial and ethnic minorities are more likely to live in poverty and have less access to healthcare and healthy food options. These factors can contribute to the development of type 2 diabetes.
- Cultural factors: Certain cultural factors can also increase the risk of developing type 2 diabetes. For example, some cultures have a diet that is high in processed foods and sugary drinks, which can contribute to weight gain and insulin resistance.
It is important to note that not all members of a particular racial or ethnic group will develop type 2 diabetes. However, it is important to be aware of the increased risk and to take steps to reduce your risk, such as maintaining a healthy weight, getting regular exercise, and eating a healthy diet.
Understanding the connection between race/ethnicity and type 2 diabetes can help us to develop more effective strategies for preventing and treating this condition.
Certain medical conditions
Certain medical conditions can increase the risk of developing type 2 diabetes. This is because these conditions can lead to insulin resistance, which is a condition in which the body does not use insulin well. Insulin resistance can lead to high blood sugar levels, which over time can damage the blood vessels and organs.
-
Polycystic Ovary Syndrome (PCOS)
PCOS is a hormonal disorder that affects women of childbearing age. Women with PCOS have high levels of androgens, which are male hormones. Androgens can interfere with insulin signaling, leading to insulin resistance and type 2 diabetes.
-
Gestational Diabetes
Gestational diabetes is a type of diabetes that develops during pregnancy. Women with gestational diabetes have high blood sugar levels during pregnancy. These high blood sugar levels can cross the placenta and reach the baby, leading to problems such as macrosomia (large birth weight) and hypoglycemia (low blood sugar) in the baby. Women with gestational diabetes are also at increased risk of developing type 2 diabetes later in life.
Other medical conditions that can increase the risk of developing type 2 diabetes include:
- Cushing’s syndrome
- Acromegaly
- Pheochromocytoma
- Hyperthyroidism
- HIV/AIDS
If you have any of these medical conditions, it is important to talk to your doctor about your risk of developing type 2 diabetes. Your doctor may recommend lifestyle changes, such as losing weight or getting more exercise, to reduce your risk.
FAQs on Type 2 Diabetes
This section addresses frequently asked questions about the causes and risk factors of Type 2 Diabetes, providing clear and concise answers for a better understanding of the condition.
Question 1: What is Type 2 Diabetes?
Type 2 Diabetes is a chronic condition that affects the body’s ability to regulate blood sugar levels. It is characterized by insulin resistance, where the body’s cells do not respond effectively to insulin, and/or a deficiency in insulin production by the pancreas.
Question 2: What are the primary causes of Type 2 Diabetes?
The exact cause of Type 2 Diabetes is not fully understood, but several factors contribute to its development, including genetics, lifestyle choices, and certain medical conditions.
Question 3: What are the common risk factors for Type 2 Diabetes?
Key risk factors for Type 2 Diabetes include obesity, physical inactivity, family history of the condition, age (over 45), certain ethnicities, and pre-existing conditions like Polycystic Ovary Syndrome (PCOS) and Gestational Diabetes.
Question 4: Can Type 2 Diabetes be prevented?
While there is no guaranteed way to prevent Type 2 Diabetes, adopting a healthy lifestyle can significantly reduce the risk. This includes maintaining a healthy weight, engaging in regular physical activity, following a balanced diet, quitting smoking, and managing stress.
Question 5: What are the complications associated with Type 2 Diabetes?
Uncontrolled Type 2 Diabetes can lead to severe complications affecting various organs and systems in the body. These may include heart disease, stroke, kidney disease, nerve damage, vision problems, and foot ulcers.
Question 6: How is Type 2 Diabetes treated?
Treatment plans for Type 2 Diabetes typically involve a combination of lifestyle modifications, oral medications, and/or insulin therapy. Regular monitoring of blood sugar levels, foot care, and management of any associated complications are also crucial aspects of diabetes care.
Remember, these FAQs provide a general overview of Type 2 Diabetes. It is essential to consult with healthcare professionals for personalized advice, diagnosis, and treatment options based on individual circumstances.
Proceed to the next section for further insights into Type 2 Diabetes.
Tips to Understand “What Causes Type 2 Diabetes”
Understanding the causes of Type 2 Diabetes is crucial for effective prevention and management of the condition. Here are some key tips to enhance your knowledge and empower yourself:
Tip 1: Explore Reputable Sources: Rely on credible health organizations, medical journals, and websites for accurate and up-to-date information on Type 2 Diabetes. Avoid relying solely on social media or unverified sources.
Tip 2: Understand Risk Factors: Familiarize yourself with the various risk factors associated with Type 2 Diabetes, such as obesity, physical inactivity, family history, age, ethnicity, and pre-existing medical conditions. Knowing your risk profile helps you make informed lifestyle choices.
Tip 3: Focus on Prevention: While genetics play a role, lifestyle modifications can significantly reduce the risk of developing Type 2 Diabetes. Prioritize maintaining a healthy weight, engaging in regular exercise, adopting a balanced diet, quitting smoking, and managing stress.
Tip 4: Recognize Symptoms: Be aware of the common symptoms of Type 2 Diabetes, including frequent urination, excessive thirst, unexplained weight loss, fatigue, and blurred vision. Early detection and diagnosis are crucial for effective management.
Tip 5: Seek Professional Advice: If you have concerns about your risk of Type 2 Diabetes or experience any symptoms, consult with a healthcare professional. They can provide personalized guidance, conduct necessary tests, and recommend appropriate treatment plans.
Remember, empowering yourself with knowledge about the causes of Type 2 Diabetes is an essential step towards prevention and optimal health. By following these tips, you can gain a deeper understanding of the condition and make informed decisions to reduce your risk and improve your well-being.
Proceed to the next section for further insights into Type 2 Diabetes.
Conclusion
Type 2 diabetes is a prevalent condition with complex causes. This article has explored the various factors that contribute to its development, including obesity, physical inactivity, family history, age, ethnicity, and certain medical conditions. Understanding these causes is paramount for effective prevention and management of the condition.
To mitigate the risk of developing Type 2 diabetes, individuals should focus on maintaining a healthy weight, engaging in regular physical activity, adopting a balanced and nutritious diet, quitting smoking, and managing stress. Early detection and diagnosis are also crucial, and people experiencing symptoms should seek medical advice promptly.
By promoting healthy lifestyle choices, raising awareness about risk factors, and supporting ongoing research, we can collectively work towards reducing the incidence and impact of Type 2 diabetes. This will not only improve the quality of life for those affected but also contribute to a healthier society overall.
Youtube Video: