Type 2 diabetes mellitus is a chronic metabolic disorder characterized by elevated blood sugar levels due to the body’s inability to effectively use insulin. Unlike type 1 diabetes, which is an autoimmune disease where the pancreas produces little to no insulin, type 2 diabetes results from insulin resistance, a condition in which the body’s cells do not respond properly to insulin.
Type 2 diabetes is a major global health concern, affecting millions of people worldwide. It is a leading cause of blindness, kidney failure, heart disease, and stroke. However, with proper management, including lifestyle modifications, medication, and regular monitoring, individuals with type 2 diabetes can live long, healthy lives.
The main article will delve deeper into the causes, symptoms, diagnosis, treatment, and prevention of type 2 diabetes mellitus. It will also discuss the latest research and advancements in diabetes management.
Type II Diabetes Mellitus
Type II diabetes mellitus is a chronic metabolic disorder characterized by elevated blood sugar levels due to the body’s inability to effectively use insulin. It is a major global health concern, affecting millions of people worldwide.
- Metabolic disorder: Type II diabetes mellitus is a disorder of the body’s metabolism, specifically the way the body uses glucose for energy.
- Elevated blood sugar: A defining characteristic of type II diabetes mellitus is persistently high blood sugar levels, also known as hyperglycemia.
- Insulin resistance: In type II diabetes mellitus, the body’s cells do not respond properly to insulin, a hormone that helps glucose enter cells for energy.
- Chronic condition: Type II diabetes mellitus is a chronic condition, meaning it lasts for a long time and requires ongoing management.
- Global health concern: Type II diabetes mellitus is a major global health concern, affecting millions of people worldwide and posing a significant burden on healthcare systems.
- Modifiable risk factors: While genetic factors play a role, type II diabetes mellitus is largely influenced by modifiable risk factors such as obesity, physical inactivity, and unhealthy diet.
These key aspects highlight the complex and multifaceted nature of type II diabetes mellitus. Understanding these aspects is crucial for effective prevention, diagnosis, and management of this condition.
Metabolic disorder
Type II diabetes mellitus is a metabolic disorder that affects the way the body uses glucose, the main source of energy for the body’s cells. In individuals with type II diabetes mellitus, the body develops insulin resistance, a condition in which the cells do not respond properly to insulin, a hormone that helps glucose enter cells for energy.
- Glucose metabolism: In healthy individuals, glucose is transported into cells with the help of insulin. However, in type II diabetes mellitus, the cells become resistant to insulin, leading to a buildup of glucose in the bloodstream.
- Insulin resistance: Insulin resistance is a hallmark of type II diabetes mellitus. It can be caused by a combination of genetic and lifestyle factors, such as obesity, physical inactivity, and unhealthy diet.
- Hyperglycemia: As glucose cannot enter cells properly due to insulin resistance, it accumulates in the bloodstream, leading to hyperglycemia, a condition of elevated blood sugar levels.
- Chronic complications: Over time, chronic hyperglycemia can damage blood vessels and organs, leading to serious complications such as heart disease, stroke, kidney failure, and blindness.
Understanding the metabolic disorder associated with type II diabetes mellitus is crucial for effective management of the condition. Lifestyle modifications, such as weight loss, regular exercise, and a healthy diet, can improve insulin sensitivity and help control blood sugar levels.
Elevated blood sugar
Elevated blood sugar is a defining characteristic of type II diabetes mellitus, a chronic metabolic disorder that affects the body’s ability to effectively use insulin. Hyperglycemia, or persistently high blood sugar levels, results from the body’s inability to properly metabolize glucose, the main source of energy for the body’s cells.
- Insulin resistance: In individuals with type II diabetes mellitus, the body’s cells become resistant to insulin, a hormone that helps glucose enter cells for energy. This resistance leads to a buildup of glucose in the bloodstream, resulting in hyperglycemia.
- Chronic complications: Over time, chronic hyperglycemia can damage blood vessels and organs, leading to serious complications such as heart disease, stroke, kidney failure, and blindness. Regular monitoring of blood sugar levels is crucial to prevent or delay the onset of these complications.
- Management strategies: Managing hyperglycemia is a cornerstone of type II diabetes mellitus management. This involves lifestyle modifications, such as weight loss, regular exercise, and a healthy diet, as well as medication to lower blood sugar levels.
- Importance of early diagnosis: Early diagnosis and intervention are crucial to prevent or delay the onset of hyperglycemia and its associated complications. Regular checkups and screening for individuals at risk of type II diabetes mellitus are essential for early detection and timely management.
Understanding the connection between elevated blood sugar and type II diabetes mellitus is paramount for effective management of the condition. Regular monitoring, lifestyle modifications, and appropriate medical care can help individuals with type II diabetes mellitus maintain healthy blood sugar levels and reduce the risk of developing serious complications.
Insulin resistance
Insulin resistance is a hallmark of type II diabetes mellitus, a chronic metabolic disorder that affects the body’s ability to effectively use insulin. Insulin is a hormone produced by the pancreas that helps glucose, the body’s main source of energy, enter cells for energy production. In individuals with type II diabetes mellitus, the body’s cells become resistant to insulin, leading to a buildup of glucose in the bloodstream, a condition known as hyperglycemia.
- Reduced glucose uptake: Insulin resistance impairs the ability of cells to take up glucose from the bloodstream. This leads to a buildup of glucose in the bloodstream, resulting in hyperglycemia.
- Metabolic complications: Insulin resistance can lead to a number of metabolic complications, including dyslipidemia (abnormal blood lipid levels) and hypertension (high blood pressure). These complications can increase the risk of cardiovascular disease, stroke, and kidney disease.
- Long-term consequences: Over time, chronic hyperglycemia can damage blood vessels and organs, leading to serious complications such as heart disease, stroke, kidney failure, and blindness.
- Management strategies: Managing insulin resistance is crucial for effective management of type II diabetes mellitus. This involves lifestyle modifications, such as weight loss, regular exercise, and a healthy diet, as well as medication to improve insulin sensitivity and lower blood sugar levels.
Insulin resistance is a complex and multifaceted condition that plays a central role in the development and progression of type II diabetes mellitus. Understanding the connection between insulin resistance and type II diabetes mellitus is essential for developing effective strategies for prevention and management of this chronic metabolic disorder.
Chronic condition
Type II diabetes mellitus is a chronic metabolic disorder that affects the body’s ability to effectively use insulin. It is characterized by elevated blood sugar levels, which can lead to serious health complications if left untreated. The chronic nature of type II diabetes mellitus means that it requires ongoing management throughout an individual’s lifetime.
There are several reasons why type II diabetes mellitus is considered a chronic condition:
- Progressive nature: Type II diabetes mellitus is a progressive disease, meaning that it tends to worsen over time. This is because the body’s cells become increasingly resistant to insulin, leading to higher and higher blood sugar levels.
- No cure: There is currently no cure for type II diabetes mellitus. However, with proper management, individuals with type II diabetes mellitus can live long, healthy lives.
- Lifelong management: Managing type II diabetes mellitus requires ongoing lifestyle modifications, such as weight loss, regular exercise, and a healthy diet. In addition, many individuals with type II diabetes mellitus require medication to lower their blood sugar levels.
Understanding the chronic nature of type II diabetes mellitus is crucial for effective management of the condition. Individuals with type II diabetes mellitus need to be aware of the importance of lifelong management and work closely with their healthcare team to develop a personalized management plan that meets their individual needs.
By understanding the connection between the chronic nature of type II diabetes mellitus and the importance of ongoing management, individuals with type II diabetes mellitus can take an active role in managing their condition and living long, healthy lives.
Global health concern
Type II diabetes mellitus is a major global health concern due to its high prevalence, increasing incidence, and significant impact on individuals and healthcare systems worldwide.
- High prevalence: Type II diabetes mellitus is one of the most prevalent chronic diseases globally, affecting an estimated 463 million people worldwide.
- Increasing incidence: The incidence of type II diabetes mellitus is rising rapidly, driven by factors such as aging populations, urbanization, and unhealthy lifestyles.
- Significant impact on individuals: Type II diabetes mellitus can lead to serious health complications, including heart disease, stroke, kidney failure, and blindness.
- Burden on healthcare systems: The management of type II diabetes mellitus and its complications places a significant burden on healthcare systems worldwide, consuming a large proportion of healthcare resources.
The global health concern of type II diabetes mellitus underscores the need for effective prevention and management strategies. Public health initiatives aimed at promoting healthy lifestyles, early detection, and appropriate treatment are crucial to reducing the burden of this disease.
Understanding the global health concern of type II diabetes mellitus is essential for healthcare professionals, policymakers, and individuals alike. By recognizing the magnitude of this issue, we can prioritize resources and efforts to address the prevention and management of type II diabetes mellitus, ultimately improving the health and well-being of millions worldwide.
Modifiable risk factors
Type II diabetes mellitus is a chronic metabolic disorder characterized by elevated blood sugar levels due to the body’s inability to effectively use insulin. While genetic factors can contribute to the development of type II diabetes mellitus, modifiable risk factors, such as obesity, physical inactivity, and unhealthy diet, play a significant role in its onset and progression.
- Obesity: Obesity is a major risk factor for type II diabetes mellitus. Excess weight, particularly abdominal fat, can lead to insulin resistance, a condition in which the body’s cells do not respond properly to insulin. Insulin resistance can lead to elevated blood sugar levels and eventually to type II diabetes mellitus.
- Physical inactivity: Physical inactivity is another significant risk factor for type II diabetes mellitus. Regular exercise helps to improve insulin sensitivity and lower blood sugar levels. Conversely, sedentary behavior can contribute to insulin resistance and increase the risk of developing type II diabetes mellitus.
- Unhealthy diet: A diet high in processed foods, sugary drinks, and unhealthy fats can contribute to weight gain and insulin resistance, both of which are risk factors for type II diabetes mellitus. Conversely, a diet rich in fruits, vegetables, and whole grains can help to maintain a healthy weight and improve insulin sensitivity.
Understanding the connection between modifiable risk factors and type II diabetes mellitus is crucial for effective prevention and management of this chronic condition. By adopting healthy lifestyle habits, such as maintaining a healthy weight, engaging in regular physical activity, and following a balanced diet, individuals can significantly reduce their risk of developing type II diabetes mellitus or improve their management of the condition if already diagnosed.
Frequently Asked Questions about Type II Diabetes Mellitus
This section addresses common questions and misconceptions surrounding type II diabetes mellitus, providing concise and informative answers.
Question 1: What is type II diabetes mellitus?
Answer: Type II diabetes mellitus is a chronic metabolic disorder characterized by elevated blood sugar levels due to the body’s inability to effectively use insulin, a hormone that helps glucose enter cells for energy.
Question 2: What are the risk factors for type II diabetes mellitus?
Answer: Modifiable risk factors include obesity, physical inactivity, and unhealthy diet. Non-modifiable risk factors include family history and age.
Question 3: What are the symptoms of type II diabetes mellitus?
Answer: Common symptoms include frequent urination, excessive thirst, unexplained weight loss, increased hunger, fatigue, and blurred vision.
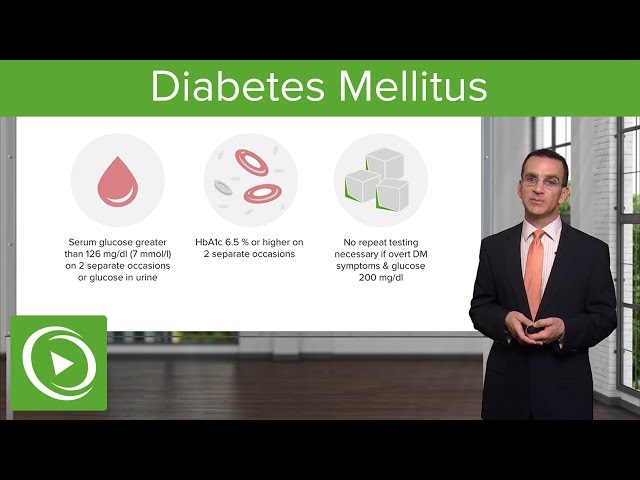
Question 4: How is type II diabetes mellitus diagnosed?
Answer: Diagnosis is typically made through blood tests that measure blood sugar levels, such as the fasting plasma glucose test or the oral glucose tolerance test.
Question 5: How is type II diabetes mellitus treated?
Answer: Treatment involves lifestyle modifications, such as weight loss, regular exercise, and a healthy diet, as well as medication to lower blood sugar levels.
Question 6: Can type II diabetes mellitus be prevented?
Answer: While there is no guaranteed way to prevent type II diabetes mellitus, adopting a healthy lifestyle can significantly reduce the risk.
In summary, understanding the nature, risk factors, symptoms, diagnosis, treatment, and prevention of type II diabetes mellitus is crucial for effective management and reducing its impact on individuals and healthcare systems worldwide.
The following section will delve into the complications associated with type II diabetes mellitus and strategies for managing them effectively.
Tips for Managing Type II Diabetes Mellitus
Type II diabetes mellitus is a chronic metabolic disorder characterized by elevated blood sugar levels due to the body’s inability to effectively use insulin. Managing type II diabetes mellitus is crucial to prevent serious health complications and maintain a good quality of life.
Tip 1: Maintain a Healthy Weight
Obesity is a major risk factor for type II diabetes mellitus. Losing weight and maintaining a healthy weight can significantly improve insulin sensitivity and blood sugar control.
Tip 2: Engage in Regular Physical Activity
Regular exercise helps to improve insulin sensitivity and lower blood sugar levels. Aim for at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous-intensity exercise per week.
Tip 3: Follow a Healthy Diet
A healthy diet for type II diabetes mellitus includes plenty of fruits, vegetables, and whole grains. Limit processed foods, sugary drinks, and unhealthy fats.
Tip 4: Monitor Blood Sugar Levels Regularly
Regular blood sugar monitoring is essential for managing type II diabetes mellitus. This allows you to track your blood sugar levels and make necessary adjustments to your treatment plan.
Tip 5: Take Medications as Prescribed
If lifestyle modifications alone are not enough to control blood sugar levels, your doctor may prescribe medication. Take your medications as directed and do not skip doses.
Tip 6: Quit Smoking
Smoking can worsen insulin resistance and increase the risk of complications from type II diabetes mellitus. Quitting smoking is one of the best things you can do for your health.
Tip 7: Manage Stress
Stress can raise blood sugar levels. Find healthy ways to manage stress, such as exercise, yoga, or meditation.
Tip 8: Get Enough Sleep
Sleep deprivation can interfere with blood sugar control. Aim for 7-8 hours of quality sleep each night.
Following these tips can help you effectively manage type II diabetes mellitus and prevent serious health complications. Remember to consult with your healthcare team for personalized guidance and support.
By adopting a healthy lifestyle and adhering to your treatment plan, you can live a full and active life with type II diabetes mellitus.
Conclusion
Type II diabetes mellitus is a chronic metabolic disorder that requires ongoing management to prevent serious health complications. Understanding the nature, risk factors, symptoms, diagnosis, treatment, and prevention of type II diabetes mellitus is crucial for effective management and reducing its impact on individuals and healthcare systems worldwide.
Adopting a healthy lifestyle, including maintaining a healthy weight, engaging in regular physical activity, and following a balanced diet, can significantly reduce the risk of developing type II diabetes mellitus or improve its management if already diagnosed. Regular blood sugar monitoring, adherence to prescribed medications, and quitting smoking are also essential for effective management. By taking a proactive approach to managing type II diabetes mellitus, individuals can live long, healthy lives.
Ongoing research and advancements in diabetes management, including new medications and technologies, offer hope for improved outcomes and a better quality of life for individuals with type II diabetes mellitus. Collaboration between healthcare professionals, researchers, and individuals with diabetes is essential to continue progress in the fight against this global health concern.
Youtube Video: