Pathophysiology of type 2 diabetes delves into the intricate mechanisms underlying the development and progression of type 2 diabetes, a prevalent chronic disease characterized by impaired glucose metabolism. This condition arises from a combination of factors, including insulin resistance, where the body’s cells fail to respond adequately to insulin, and impaired insulin secretion by the pancreas.
Understanding the pathophysiology of type 2 diabetes is crucial for effective management and prevention strategies. By deciphering the complex interplay of metabolic pathways, genetic predisposition, and environmental influences, researchers and healthcare professionals can develop targeted interventions to mitigate the impact of this debilitating disease.
This article explores the multifaceted pathophysiology of type 2 diabetes, examining the cellular and molecular mechanisms that contribute to its development. We will delve into the role of insulin resistance, pancreatic beta-cell dysfunction, and the interplay of genetic and environmental factors in the progression of this condition.
Pathophysiology of Type 2 Diabetes
Understanding the pathophysiology of type 2 diabetes is crucial for effective management and prevention. Key aspects include:
- Insulin resistance
- Pancreatic beta-cell dysfunction
- Genetic predisposition
- Obesity
- Inflammation
- Metabolic dysregulation
- Environmental factors
- Epigenetic modifications
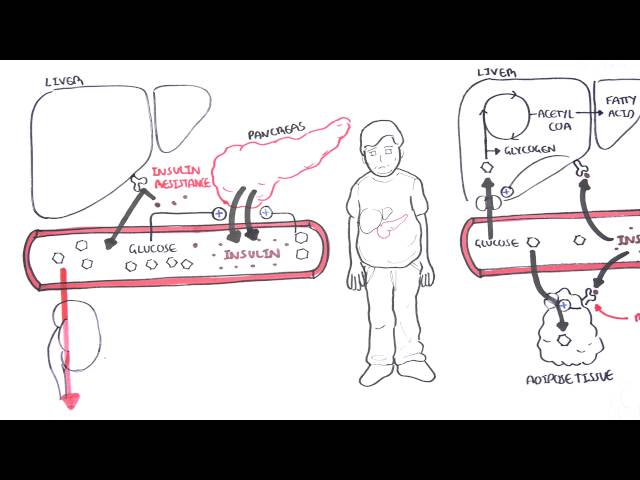
Insulin resistance, a hallmark of type 2 diabetes, arises when cells fail to respond adequately to insulin, leading to impaired glucose uptake. Pancreatic beta-cell dysfunction, another key aspect, involves the failure of these cells to produce and secrete sufficient insulin. Genetic predisposition plays a significant role, with certain genetic variants increasing the risk of developing type 2 diabetes. Obesity, a major risk factor, contributes to insulin resistance and metabolic dysregulation. Inflammation, often associated with obesity, can impair insulin signaling and promote beta-cell dysfunction. Environmental factors, such as sedentary lifestyle and unhealthy diet, can also contribute to the development of type 2 diabetes. Epigenetic modifications, influenced by environmental factors, can alter gene expression and contribute to disease progression.
Insulin Resistance
Insulin resistance is a fundamental aspect of the pathophysiology of type 2 diabetes, characterized by the body’s inability to respond effectively to insulin, a hormone that regulates glucose metabolism. This impaired response leads to reduced glucose uptake and utilization by cells, resulting in elevated blood glucose levels.
- Cellular Mechanisms: Insulin resistance involves defects in insulin signaling pathways within cells. Insulin binds to specific receptors on the cell surface, triggering a cascade of events that promote glucose uptake and metabolism. However, in insulin resistance, these signaling pathways are impaired, leading to decreased glucose transport into cells.
- Adipose Tissue Dysfunction: Adipose tissue plays a crucial role in insulin resistance. In obesity, excessive fat accumulation leads to the dysfunction of adipose tissue, resulting in increased inflammation and the release of adipokines, signaling molecules that impair insulin signaling.
- Ectopic Fat Deposition: Insulin resistance can also arise from the deposition of fat in non-adipose tissues, such as the liver and muscle. This ectopic fat accumulation disrupts normal cellular function and impairs insulin signaling.
- Genetic Factors: Genetic predisposition plays a role in insulin resistance. Certain genetic variants have been linked to impaired insulin signaling and increased risk of developing type 2 diabetes.
Insulin resistance is a complex and multifaceted condition that significantly contributes to the development of type 2 diabetes. Understanding its underlying cellular and molecular mechanisms is crucial for devising effective strategies to prevent and manage this prevalent metabolic disorder.
Pancreatic Beta-Cell Dysfunction
Pancreatic beta-cell dysfunction is a pivotal aspect of the pathophysiology of type 2 diabetes, characterized by the impaired ability of these cells to produce and secrete insulin, a critical hormone for glucose homeostasis. This dysfunction contributes significantly to the development and progression of type 2 diabetes.
-
Reduced Insulin Production:
In type 2 diabetes, pancreatic beta-cells lose their ability to produce sufficient insulin. This diminished insulin production stems from various factors, including cellular stress, oxidative damage, and impaired gene expression. As a result, the body cannot meet its insulin requirements, leading to impaired glucose metabolism.
-
Defective Insulin Secretion:
Even when beta-cells produce insulin, its secretion can be impaired in type 2 diabetes. This secretory defect arises from disruptions in the signaling pathways that trigger insulin release. Consequently, insulin is not released appropriately in response to elevated glucose levels, further exacerbating hyperglycemia.
-
Beta-Cell Mass Loss:
Over time, prolonged stress and dysfunction can lead to the loss of beta-cell mass in type 2 diabetes. This reduction in beta-cell number further diminishes insulin production capacity and contributes to the progressive nature of the disease.
-
Genetic Predisposition:
Genetic factors also play a role in pancreatic beta-cell dysfunction. Certain genetic variants have been associated with an increased risk of developing type 2 diabetes by impairing beta-cell function and survival.
Pancreatic beta-cell dysfunction is a complex and multifaceted process that significantly contributes to the pathophysiology of type 2 diabetes. Understanding the underlying mechanisms of this dysfunction is crucial for developing effective therapeutic strategies aimed at preserving beta-cell function and improving glucose control.
Genetic Predisposition and the Pathophysiology of Type 2 Diabetes
Genetic predisposition plays a significant role in the pathophysiology of type 2 diabetes, a complex metabolic disorder characterized by impaired insulin action and secretion. This genetic influence stems from variations in specific genes that can increase an individual’s susceptibility to developing the condition.
-
MODY Genes:
Mutations in genes responsible for beta-cell function, known as MODY (maturity-onset diabetes of the young) genes, can lead to impaired insulin secretion. These mutations disrupt the normal development and function of beta-cells, resulting in reduced insulin production and an increased risk of type 2 diabetes.
-
Insulin Receptor Gene:
Variations in the insulin receptor gene can affect insulin signaling pathways. Mutations in this gene can lead to insulin resistance, a condition in which cells fail to respond adequately to insulin, resulting in impaired glucose uptake and utilization.
-
Transcription Factors:
Transcription factors are proteins that regulate gene expression. Alterations in genes encoding transcription factors involved in beta-cell development and function can disrupt the normal production and secretion of insulin, contributing to the development of type 2 diabetes.
-
Genome-Wide Association Studies:
Genome-wide association studies (GWAS) have identified numerous genetic variants associated with an increased risk of type 2 diabetes. These variants are often found in genes involved in insulin signaling, beta-cell function, and glucose metabolism. By studying these genetic variations, researchers aim to better understand the genetic basis of type 2 diabetes and develop more targeted therapies.
Understanding the genetic predisposition to type 2 diabetes is crucial for developing personalized prevention and treatment strategies. By identifying individuals at high risk, healthcare professionals can implement early interventions, such as lifestyle modifications and closer monitoring, to delay or prevent the onset of the disease.
Obesity
Obesity is a significant risk factor for the development of type 2 diabetes, with a strong correlation between the two conditions. Obesity leads to a complex interplay of metabolic and hormonal changes that contribute to the pathophysiology of type 2 diabetes.
Excessive adipose tissue, a hallmark of obesity, releases various hormones and signaling molecules, known as adipokines, which have systemic effects on metabolism. Adipokines such as leptin and resistin can impair insulin signaling, leading to insulin resistance, a key feature of type 2 diabetes. Additionally, obesity promotes inflammation, which further disrupts insulin signaling and exacerbates insulin resistance.
Adipose tissue dysfunction in obesity also leads to increased production of free fatty acids, which can accumulate in the liver and muscle, contributing to insulin resistance and impaired glucose metabolism. Furthermore, obesity can cause mechanical stress on pancreatic beta-cells, affecting their function and insulin secretion, ultimately leading to pancreatic beta-cell failure.
Understanding the connection between obesity and the pathophysiology of type 2 diabetes is crucial for developing effective prevention and management strategies. Lifestyle interventions aimed at weight loss and maintaining a healthy weight can significantly reduce the risk of developing type 2 diabetes or improve its management in individuals who already have the condition.
Inflammation
Inflammation plays a pivotal role in the pathophysiology of type 2 diabetes, contributing to its development and progression. This chronic, low-grade inflammation is characterized by the activation of immune cells and the release of inflammatory mediators, which can disrupt insulin signaling and impair glucose metabolism.
Adipose tissue, a major source of inflammation in obesity, releases various pro-inflammatory adipokines, such as tumor necrosis factor-alpha (TNF-) and interleukin-6 (IL-6), which can interfere with insulin signaling in target tissues. This impaired insulin signaling leads to insulin resistance, a hallmark of type 2 diabetes.
Inflammation can also directly affect pancreatic beta-cells, which are responsible for producing insulin. Inflammatory mediators can induce beta-cell dysfunction and apoptosis, contributing to the decline in insulin production observed in type 2 diabetes. Additionally, inflammation can promote the development of oxidative stress, further damaging beta-cells and exacerbating insulin deficiency.
Understanding the connection between inflammation and the pathophysiology of type 2 diabetes is crucial for developing effective therapeutic strategies. Anti-inflammatory interventions that target specific inflammatory mediators or pathways may offer novel approaches to prevent or treat type 2 diabetes.
Metabolic dysregulation
Metabolic dysregulation is a central aspect of the pathophysiology of type 2 diabetes, characterized by disturbances in the body’s ability to metabolize and utilize glucose effectively. This dysregulation encompasses multiple facets, each contributing to the development and progression of the disease.
- Insulin Resistance and Impaired Glucose Uptake: Insulin resistance, a key feature of type 2 diabetes, arises when cells fail to respond adequately to insulin, the hormone responsible for facilitating glucose uptake. This impaired glucose uptake leads to elevated blood glucose levels and contributes to the metabolic dysregulation observed in the disease.
- Defective Insulin Secretion: In type 2 diabetes, pancreatic beta-cells, responsible for producing and secreting insulin, may exhibit impaired function. This can result in insufficient insulin production or an inability to secrete insulin appropriately in response to elevated glucose levels, further exacerbating metabolic dysregulation and hyperglycemia.
- Dysregulation of Gluconeogenesis and Glycogenolysis: Gluconeogenesis, the production of glucose from non-carbohydrate sources, and glycogenolysis, the breakdown of glycogen into glucose, are processes that contribute to maintaining blood glucose homeostasis. In type 2 diabetes, these processes may become dysregulated, leading to excessive glucose production and contributing to hyperglycemia.
- Altered Lipid Metabolism: Metabolic dysregulation in type 2 diabetes also extends to lipid metabolism. Individuals with the condition often exhibit elevated levels of triglycerides and low levels of high-density lipoprotein (HDL) cholesterol, contributing to the increased risk of cardiovascular complications associated with diabetes.
Understanding the multifaceted nature of metabolic dysregulation in type 2 diabetes is crucial for developing effective strategies to prevent and manage the disease. By addressing the underlying metabolic disturbances, therapeutic interventions can aim to improve insulin sensitivity, restore appropriate insulin secretion, and normalize glucose metabolism, ultimately leading to improved health outcomes.
Environmental factors
Environmental factors play a significant role in the pathophysiology of type 2 diabetes, interacting with genetic and biological determinants to influence the development and progression of the disease. These factors encompass a wide range of elements that can impact metabolic processes and contribute to the underlying mechanisms of type 2 diabetes.
- Diet and Nutrition: Dietary patterns high in processed foods, sugary drinks, and unhealthy fats can contribute to weight gain and obesity, which are major risk factors for type 2 diabetes. Additionally, diets low in fiber and whole grains can impair glucose metabolism and insulin sensitivity.
- Physical Inactivity: Sedentary lifestyles and lack of regular physical activity can lead to decreased insulin sensitivity and impaired glucose tolerance, increasing the risk of developing type 2 diabetes. Exercise, on the other hand, improves insulin sensitivity and promotes glucose utilization.
- Smoking: Smoking is a significant environmental risk factor for type 2 diabetes. Exposure to cigarette smoke increases oxidative stress and inflammation, which can damage pancreatic beta-cells and impair insulin secretion.
- Air Pollution: Exposure to air pollutants, particularly particulate matter and nitrogen oxides, has been linked to an increased risk of developing type 2 diabetes. These pollutants can induce inflammation and oxidative stress, affecting glucose metabolism and insulin sensitivity.
Understanding the multifaceted impact of environmental factors on the pathophysiology of type 2 diabetes is crucial for developing comprehensive prevention and management strategies. By addressing modifiable environmental factors, individuals can reduce their risk of developing type 2 diabetes or improve its management if already diagnosed.
Epigenetic modifications
Epigenetic modifications play a crucial role in the pathophysiology of type 2 diabetes, a complex metabolic disorder characterized by insulin resistance and impaired insulin secretion. Epigenetic modifications are mitotically heritable changes in gene expression that do not involve alterations in the DNA sequence itself. These modifications can influence gene expression by affecting chromatin structure and accessibility, thereby regulating the transcription of specific genes.
In the context of type 2 diabetes, epigenetic modifications have been implicated in both the development and progression of the disease. Environmental factors, such as diet, physical activity, and exposure to toxins, can induce epigenetic changes that alter the expression of genes involved in glucose metabolism and insulin signaling. For instance, high-fat diets have been shown to promote epigenetic modifications that lead to decreased insulin sensitivity, while exercise has been associated with epigenetic changes that improve insulin action.
Understanding the role of epigenetic modifications in type 2 diabetes has significant practical implications. By identifying specific epigenetic modifications that contribute to the disease, researchers can develop targeted therapies aimed at reversing or preventing these changes. Additionally, lifestyle interventions that promote favorable epigenetic modifications, such as regular exercise and a healthy diet, can be recommended for individuals at risk of or with type 2 diabetes.
FAQs on Pathophysiology of Type 2 Diabetes
What is the pathophysiology of type 2 diabetes?
Type 2 diabetes is characterized by insulin resistance, where cells fail to respond adequately to insulin, and impaired insulin secretion by the pancreas. This leads to elevated blood glucose levels and can result in long-term complications if left untreated.
Question 1: What are the key factors contributing to the development of type 2 diabetes?
Obesity, physical inactivity, unhealthy diet, and family history are significant risk factors for developing type 2 diabetes. Additionally, certain genetic predispositions and environmental factors can also play a role.
Question 2: How does insulin resistance occur in type 2 diabetes?
Insulin resistance arises when cells, particularly muscle, fat, and liver cells, become less responsive to the effects of insulin. This impaired response leads to decreased glucose uptake and utilization, resulting in elevated blood glucose levels.
Question 3: What is the role of pancreatic beta cells in type 2 diabetes?
Pancreatic beta cells are responsible for producing and secreting insulin. In type 2 diabetes, beta cells may become dysfunctional, leading to impaired insulin secretion and contributing to hyperglycemia.
Question 4: How does inflammation contribute to the pathophysiology of type 2 diabetes?
Chronic inflammation is associated with insulin resistance and impaired glucose metabolism. Adipose tissue dysfunction and the release of pro-inflammatory adipokines can contribute to the development and progression of type 2 diabetes.
Question 5: What are the potential long-term complications of type 2 diabetes?
Uncontrolled type 2 diabetes can lead to various complications, including cardiovascular disease, stroke, kidney disease, nerve damage, and eye problems. Early diagnosis and proper management are crucial to prevent or delay these complications.
Question 6: How can lifestyle modifications impact the pathophysiology of type 2 diabetes?
Adopting a healthy lifestyle, including regular exercise, a balanced diet, and maintaining a healthy weight, can improve insulin sensitivity, reduce inflammation, and promote better blood glucose control in individuals with type 2 diabetes.
Understanding the pathophysiology of type 2 diabetes is essential for developing effective prevention and management strategies. By addressing modifiable risk factors and implementing appropriate interventions, individuals can improve their overall health outcomes and reduce the risk of developing or experiencing complications related to type 2 diabetes.
Transition to the next article section: Exploring Treatment Options for Type 2 Diabetes
Understanding Pathophysiology of Type 2 Diabetes
Understanding the pathophysiology of type 2 diabetes is crucial for healthcare professionals and individuals alike. It provides a foundation for developing effective strategies to prevent, manage, and treat this prevalent condition. Here are some key tips to enhance your understanding:
Tip 1: Grasp the Core Mechanisms
Delve into the fundamental mechanisms underlying type 2 diabetes, including insulin resistance, impaired insulin secretion, and their impact on glucose metabolism. Tip 2: Recognize the Role of Pancreatic Beta Cells
Comprehend the crucial role of pancreatic beta cells in producing and secreting insulin, and how their dysfunction contributes to the development of type 2 diabetes. Tip 3: Identify the Significance of Insulin Resistance
Understand the process of insulin resistance, where cells become less responsive to insulin, leading to impaired glucose uptake and utilization. Tip 4: Explore the Impact of Genetic Predisposition
Examine the genetic factors that can increase an individual’s susceptibility to developing type 2 diabetes and how they influence disease progression. Tip 5: Consider the Influence of Environmental Factors
Recognize the impact of environmental factors, such as diet, physical activity, and exposure to toxins, on the pathophysiology of type 2 diabetes. Tip 6: Appreciate the Role of Inflammation
Understand how chronic inflammation contributes to insulin resistance and impaired glucose metabolism, and its implications for the development of type 2 diabetes. Tip 7: Stay Updated on Research Advancements
Keep abreast of ongoing research in the field of type 2 diabetes pathophysiology to stay informed about the latest discoveries and potential therapeutic approaches.
By incorporating these tips into your knowledge base, you will gain a comprehensive understanding of the pathophysiology of type 2 diabetes. This understanding empowers you to make informed decisions regarding prevention, management, and treatment strategies.
Conclusion: Understanding the pathophysiology of type 2 diabetes is an essential step towards effectively addressing the global health burden of this condition. Through a deeper understanding of the underlying mechanisms, healthcare professionals can personalize treatment plans, empowering individuals to manage their condition and improve their overall well-being.
Conclusion
Type 2 diabetes is a complex metabolic disorder with a multifactorial pathophysiology involving insulin resistance, impaired insulin secretion, and the interplay of genetic, environmental, and lifestyle factors. Understanding the intricacies of this pathophysiology is paramount for developing comprehensive strategies to prevent, diagnose, and manage type 2 diabetes effectively.
By elucidating the underlying mechanisms, researchers and healthcare professionals can tailor individualized treatment plans that target specific pathophysiological pathways. This precision approach holds the key to improving patient outcomes, reducing the risk of complications, and ultimately enhancing the quality of life for those affected by type 2 diabetes.
Youtube Video: