Pathophysiology of Diabetes refers to the physiological processes underlying the development and progression of diabetes mellitus, a group of metabolic disorders characterized by elevated blood glucose levels. In type 1 diabetes, the body’s immune system destroys the insulin-producing beta cells in the pancreas, leading to an absolute deficiency of insulin. In type 2 diabetes, the body becomes resistant to insulin, and the pancreas is unable to produce enough insulin to overcome this resistance. Both types of diabetes result in chronic hyperglycemia, which can damage various organs and tissues over time.
Understanding the pathophysiology of diabetes is crucial for developing effective treatments and preventive strategies. Historically, diabetes was a devastating disease with limited treatment options. However, advancements in medical research have led to a better understanding of the disease process and the development of various medications and therapies that can help manage blood glucose levels and prevent complications.
The main article will delve into the specific mechanisms involved in the pathophysiology of diabetes, including the role of genetics, environmental factors, and lifestyle choices. It will also discuss the different types of diabetes, their symptoms, diagnosis, and treatment approaches.
Pathophysiology of Diabetes
The pathophysiology of diabetes, the study of the physiological processes underlying the development and progression of diabetes mellitus, involves several key aspects:
- Insulin resistance: The body’s cells become less responsive to insulin, leading to elevated blood glucose levels.
- Beta-cell dysfunction: The pancreas produces less insulin, or the insulin it produces is less effective.
- Hyperglycemia: Chronically elevated blood glucose levels.
- Glycation: The non-enzymatic attachment of glucose to proteins and lipids, leading to tissue damage.
- Inflammation: Chronic inflammation plays a role in the development and progression of diabetes.
- Oxidative stress: An imbalance between the production of reactive oxygen species and the body’s ability to counteract their harmful effects.
- Genetic factors: Certain genetic variants increase the risk of developing diabetes.
These key aspects are interconnected and contribute to the development and progression of diabetes. For example, insulin resistance leads to hyperglycemia, which in turn can damage the beta-cells and further impair insulin production. Inflammation and oxidative stress can also contribute to beta-cell dysfunction and insulin resistance. Understanding these pathophysiological processes is crucial for developing effective treatments and preventive strategies for diabetes.
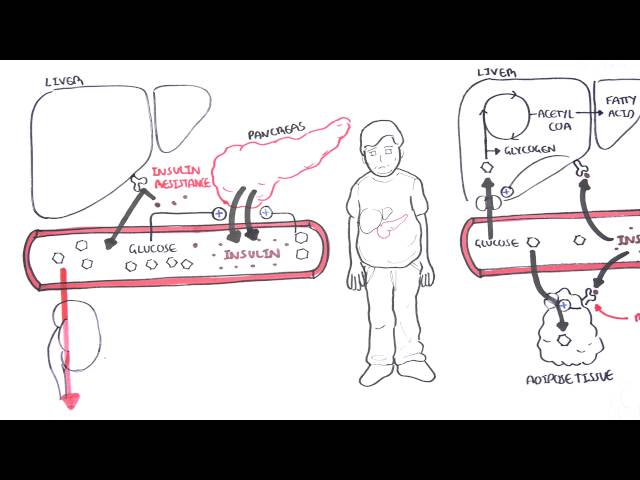
Insulin resistance
Insulin resistance is a key component in the pathophysiology of diabetes, particularly in type 2 diabetes. When the body’s cells become less responsive to insulin, glucose cannot enter the cells as easily, leading to elevated blood glucose levels. This can have several implications:
- Increased glucose production by the liver: Insulin normally suppresses glucose production by the liver. However, in insulin resistance, the liver continues to produce glucose, contributing to hyperglycemia.
- Decreased glucose uptake by muscles and fat: Insulin stimulates glucose uptake by muscles and fat cells. In insulin resistance, glucose uptake is impaired, leading to further elevation of blood glucose levels.
- Increased inflammation: Insulin resistance is associated with chronic inflammation, which can contribute to insulin resistance and beta-cell dysfunction.
- Oxidative stress: Insulin resistance can lead to increased oxidative stress, which can damage cells and contribute to the development of diabetes complications.
Understanding the role of insulin resistance in the pathophysiology of diabetes is crucial for developing effective treatments and preventive strategies. Lifestyle interventions, such as exercise and weight loss, can improve insulin sensitivity and reduce the risk of developing type 2 diabetes. Additionally, medications that increase insulin sensitivity or decrease glucose production can be used to manage blood glucose levels in people with diabetes.
Beta-cell dysfunction
Beta-cell dysfunction plays a central role in the pathophysiology of diabetes, particularly in type 1 and type 2 diabetes. Beta-cells are responsible for producing insulin, a hormone that regulates blood glucose levels. When beta-cells are damaged or dysfunctional, they cannot produce enough insulin, or the insulin they produce is less effective, leading to elevated blood glucose levels.
- Autoimmune destruction: In type 1 diabetes, the immune system mistakenly attacks and destroys beta-cells, leading to a severe deficiency of insulin.
- Glucotoxicity: Chronically elevated blood glucose levels can damage beta-cells, impairing their ability to produce insulin.
- Inflammation: Chronic inflammation can contribute to beta-cell dysfunction and death.
- Genetic factors: Certain genetic variants can increase the risk of beta-cell dysfunction and diabetes.
Beta-cell dysfunction is a major factor in the development and progression of diabetes. Understanding the mechanisms underlying beta-cell dysfunction is crucial for developing effective treatments and preventive strategies for diabetes.
Hyperglycemia
Hyperglycemia, or chronically elevated blood glucose levels, is a central component of the pathophysiology of diabetes. It is a result of either the body’s inability to produce enough insulin (type 1 diabetes) or the body’s resistance to insulin’s effects (type 2 diabetes). Hyperglycemia can have a wide range of effects on the body, including:
- Damage to blood vessels: Chronically elevated blood glucose levels can damage the blood vessels, leading to complications such as heart disease, stroke, and kidney disease.
- Nerve damage: Hyperglycemia can also damage nerves, leading to numbness, tingling, and pain in the hands and feet.
- Eye damage: Hyperglycemia can damage the blood vessels in the retina, leading to vision problems and blindness.
- Increased risk of infection: Hyperglycemia can weaken the immune system, increasing the risk of infections.
Understanding the connection between hyperglycemia and the pathophysiology of diabetes is crucial for developing effective treatments and preventive strategies. Managing blood glucose levels is essential for preventing or delaying the complications of diabetes. This can be achieved through lifestyle interventions, such as exercise and weight loss, and medications that lower blood glucose levels.
In conclusion, hyperglycemia is a key component of the pathophysiology of diabetes and is responsible for many of the complications associated with the disease. Managing blood glucose levels is essential for preventing or delaying these complications and improving the overall health of people with diabetes.
Glycation
Glycation is a complex process that occurs when glucose molecules attach to proteins and lipids in the body. This process is accelerated in people with diabetes, who have chronically elevated blood glucose levels. Glycation can lead to the formation of advanced glycation end products (AGEs), which are harmful compounds that can damage tissues and organs throughout the body.
In the context of diabetes, glycation plays a significant role in the development and progression of the disease’s complications. For example, glycation of proteins in the blood vessels can lead to thickening and stiffening of the arteries, which can increase the risk of heart disease and stroke. Glycation of proteins in the kidneys can lead to kidney damage and failure. Glycation of proteins in the eyes can lead to cataracts and other vision problems. In the nervous system, glycation can damage nerves, leading to numbness, tingling, and pain.
Understanding the role of glycation in the pathophysiology of diabetes is crucial for developing effective treatments and preventive strategies. Managing blood glucose levels is essential for preventing or delaying the development of complications. Additionally, medications and lifestyle interventions that reduce glycation may also be beneficial for people with diabetes.
In conclusion, glycation is a major contributor to the pathophysiology of diabetes and its complications. Understanding the mechanisms underlying glycation is essential for developing effective strategies to prevent and treat diabetes.
Inflammation
Inflammation is a complex biological process that plays a crucial role in the body’s response to injury, infection, and disease. However, chronic inflammation can contribute to the development and progression of various diseases, including diabetes.
- Adipose tissue inflammation: Adipose tissue, or body fat, is an important site of inflammation in obesity and type 2 diabetes. Adipose tissue secretes inflammatory cytokines, which can contribute to insulin resistance and beta-cell dysfunction.
- Islet inflammation: The islets of Langerhans in the pancreas contain beta-cells, which produce insulin. In type 1 diabetes, islet inflammation leads to the destruction of beta-cells and insulin deficiency. In type 2 diabetes, islet inflammation can contribute to beta-cell dysfunction and insulin resistance.
- Systemic inflammation: Chronic inflammation can also occur in other parts of the body, such as the blood vessels and liver. Systemic inflammation can contribute to insulin resistance, beta-cell dysfunction, and the development of diabetes complications.
- Genetic factors: Certain genetic variants can increase the risk of developing chronic inflammation and diabetes. For example, variations in the genes encoding inflammatory cytokines have been linked to an increased risk of type 2 diabetes.
Understanding the connection between inflammation and the pathophysiology of diabetes is crucial for developing effective treatments and preventive strategies. Lifestyle interventions, such as exercise and weight loss, can reduce inflammation and improve insulin sensitivity. Additionally, medications that target specific inflammatory pathways may be beneficial for people with diabetes.
In conclusion, chronic inflammation plays a significant role in the development and progression of diabetes. Understanding the mechanisms underlying this connection is essential for developing comprehensive strategies to prevent and treat diabetes.
Oxidative stress
Oxidative stress plays a significant role in the pathophysiology of diabetes. Reactive oxygen species (ROS) are produced as a byproduct of cellular metabolism, and they can damage cellular components such as DNA, proteins, and lipids. In diabetes, hyperglycemia leads to increased production of ROS, while the body’s antioxidant defenses are impaired. This imbalance between ROS production and antioxidant defenses leads to oxidative stress, which contributes to the development and progression of diabetes complications.
Oxidative stress can damage beta-cells, leading to impaired insulin production. It can also promote insulin resistance and inflammation, further exacerbating hyperglycemia. Additionally, oxidative stress can contribute to the development of diabetic complications such as cardiovascular disease, nephropathy, and retinopathy. For example, oxidative stress can damage the blood vessels, leading to atherosclerosis and heart disease. It can also damage the kidneys, leading to nephropathy and kidney failure. Oxidative stress can also damage the retina, leading to retinopathy and vision loss.
Understanding the connection between oxidative stress and the pathophysiology of diabetes is crucial for developing effective treatments and preventive strategies. Lifestyle interventions, such as exercise and weight loss, can reduce oxidative stress and improve insulin sensitivity. Additionally, medications that target oxidative stress may be beneficial for people with diabetes.
In conclusion, oxidative stress is a major contributor to the pathophysiology of diabetes and its complications. Understanding the mechanisms underlying this connection is essential for developing comprehensive strategies to prevent and treat diabetes.
Genetic factors
Genetic factors play a significant role in the pathophysiology of diabetes. Certain genetic variants can increase the risk of developing type 1 or type 2 diabetes. These genetic variants can affect the function of beta-cells, insulin sensitivity, and other aspects of glucose metabolism.
- Variants in genes encoding insulin and its receptors: These variants can affect the production, secretion, or action of insulin, leading to insulin resistance or beta-cell dysfunction.
- Variants in genes involved in beta-cell development and function: These variants can affect the formation, growth, and function of beta-cells, leading to impaired insulin production.
- Variants in genes involved in glucose metabolism: These variants can affect the transport, utilization, or storage of glucose, leading to hyperglycemia.
- Variants in genes involved in immune function: These variants can affect the immune system’s response to beta-cells, leading to the development of type 1 diabetes.
Understanding the connection between genetic factors and the pathophysiology of diabetes is crucial for developing effective preventive and therapeutic strategies. Genetic testing can be used to identify individuals at high risk of developing diabetes, allowing for early intervention and lifestyle modifications. Additionally, research into the genetic basis of diabetes may lead to the development of novel treatments that target specific genetic variants.
FAQs
This section provides answers to frequently asked questions regarding the pathophysiology of diabetes, a group of metabolic disorders characterized by elevated blood glucose levels. These questions address common concerns or misconceptions, offering concise yet informative explanations.
Question 1: What is the primary mechanism underlying insulin resistance in type 2 diabetes?
In type 2 diabetes, the body’s cells become less responsive to insulin, leading to impaired glucose uptake and elevated blood sugar levels. This insulin resistance can result from various factors, including obesity, physical inactivity, and genetic predisposition.
Question 2: How does hyperglycemia contribute to the development of diabetes complications?
Chronically elevated blood glucose levels can damage blood vessels and nerves throughout the body, increasing the risk of complications such as heart disease, stroke, kidney disease, and neuropathy. Hyperglycemia also impairs the immune system, making individuals more susceptible to infections.
Question 3: What role does inflammation play in the pathophysiology of diabetes?
Chronic inflammation is associated with both type 1 and type 2 diabetes. Adipose tissue inflammation, islet inflammation, and systemic inflammation can contribute to insulin resistance, beta-cell dysfunction, and the development of diabetes complications.
Question 4: How does oxidative stress impact beta-cell function in diabetes?
Oxidative stress occurs when there is an imbalance between the production of reactive oxygen species (ROS) and the body’s antioxidant defenses. In diabetes, hyperglycemia leads to increased ROS production, which can damage beta-cells and impair insulin production.
Question 5: Are there genetic factors that influence the risk of developing diabetes?
Yes, certain genetic variants can increase the risk of developing type 1 or type 2 diabetes. These genetic variants can affect beta-cell function, insulin sensitivity, and other aspects of glucose metabolism.
Question 6: Can lifestyle modifications impact the pathophysiology of diabetes?
Lifestyle modifications, such as exercise, weight loss, and a healthy diet, can improve insulin sensitivity, reduce inflammation, and lower blood glucose levels. These interventions can help prevent or delay the development and progression of diabetes and its complications.
Understanding the pathophysiology of diabetes is crucial for developing effective preventive and therapeutic strategies. By addressing these frequently asked questions, we aim to provide a deeper understanding of the underlying mechanisms and risk factors associated with diabetes.
To learn more about the pathophysiology of diabetes, please refer to the following article sections:
Tips for Managing the Pathophysiology of Diabetes
Understanding the pathophysiology of diabetes, the physiological processes underlying the development and progression of the disease, is essential for effective management. Here are five tips to help you manage the pathophysiology of diabetes:
Tip 1: Control Blood Glucose Levels
Maintaining blood glucose levels within a healthy range is crucial for preventing or delaying the complications of diabetes. This can be achieved through lifestyle modifications, such as regular exercise, a healthy diet, and weight management. Medications may also be necessary to lower blood glucose levels.
Tip 2: Improve Insulin Sensitivity
Insulin resistance is a major factor in the development of type 2 diabetes. Improving insulin sensitivity helps the body use insulin more effectively, which can lower blood glucose levels. Exercise, weight loss, and certain medications can improve insulin sensitivity.
Tip 3: Reduce Inflammation
Chronic inflammation plays a role in the development and progression of diabetes. Reducing inflammation can help improve insulin sensitivity and beta-cell function. Lifestyle modifications, such as a healthy diet and regular exercise, can help reduce inflammation. Anti-inflammatory medications may also be beneficial.
Tip 4: Protect Beta-Cells
Beta-cells are responsible for producing insulin. Protecting beta-cells from damage is crucial for preventing or delaying the development of type 1 diabetes and preserving insulin production in type 2 diabetes. Certain medications and lifestyle modifications, such as avoiding smoking and maintaining a healthy weight, can help protect beta-cells.
Tip 5: Manage Oxidative Stress
Oxidative stress can damage beta-cells and contribute to the development of diabetes complications. Managing oxidative stress can help protect beta-cells and reduce the risk of complications. Lifestyle modifications, such as regular exercise and a diet rich in antioxidants, can help manage oxidative stress.
By following these tips, you can effectively manage the pathophysiology of diabetes and prevent or delay the development of complications.
Remember to consult with your healthcare provider for personalized advice and treatment options. Together, you can develop a comprehensive plan to manage your diabetes and improve your overall health.
Conclusion
The pathophysiology of diabetes, encompassing the intricate physiological processes underlying the development and progression of the disease, has been extensively explored in this article. We have examined the key aspects of diabetes pathophysiology, including insulin resistance, beta-cell dysfunction, hyperglycemia, glycation, inflammation, oxidative stress, and genetic factors.
Understanding the pathophysiology of diabetes is not merely an academic pursuit; it holds immense practical significance in guiding clinical practice and shaping preventive strategies. By unraveling the complex mechanisms involved, we gain insights into the disease’s progression and identify potential targets for therapeutic intervention. Moreover, this knowledge empowers individuals with diabetes to make informed decisions about their health management, enabling them to lead fulfilling lives.
Youtube Video: