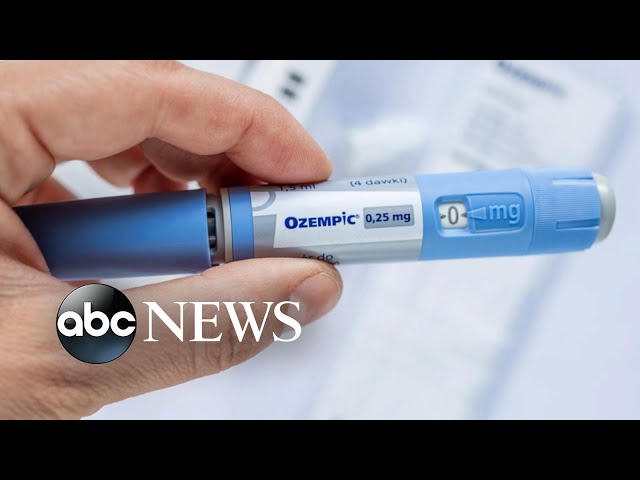
A diabetic shot is a type of injection therapy commonly administered by individuals diagnosed with diabetes to regulate their blood sugar levels. It involves the subcutaneous administration of insulin or other glucose-lowering medications. Insulin is a hormone produced by the pancreas to aid the absorption of glucose into cells for energy. Diabetic shots supplement or replace the insulin that the body is unable to produce or effectively utilize.
Diabetic shots are crucial for managing blood sugar levels, preventing complications such as hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar), and reducing the risk of long-term health issues like heart disease, stroke, kidney disease, and nerve damage. Historically, diabetic shots were the primary treatment for diabetes, but nowadays, they are often combined with other medications, lifestyle modifications, and technological advancements.
The main article will delve into the types of diabetic shots available, their administration methods, the benefits and risks associated with each type, and the latest innovations in diabetic shot therapy.
diabetic shot
A diabetic shot, also known as insulin injection therapy, is a crucial aspect of diabetes management. It plays a vital role in regulating blood sugar levels and preventing complications. Key aspects of diabetic shots include:
- Insulin: The hormone administered via injection to facilitate glucose absorption.
- Subcutaneous: The method of injection, where medication is delivered just beneath the skin.
- Blood sugar control: The primary purpose of diabetic shots, helping individuals manage their blood glucose levels.
- Complication prevention: Diabetic shots aid in preventing long-term complications associated with diabetes, such as heart disease and kidney damage.
- Medication options: Various types of insulin and other glucose-lowering medications are available for diabetic shots, tailored to individual needs.
- Technological advancements: Innovations like insulin pumps and continuous glucose monitors enhance the precision and convenience of diabetic shot therapy.
In summary, diabetic shots involve the injection of insulin or other medications to regulate blood sugar levels. They are essential for managing diabetes, preventing complications, and improving the overall health and well-being of individuals with this condition. The various aspects of diabetic shots, from the type of insulin used to the technological advancements in delivery methods, contribute to their effectiveness in diabetes management.
Insulin
Insulin is a hormone naturally produced by the pancreas to regulate blood sugar levels. It acts as a key that unlocks cells, allowing glucose to enter and be utilized for energy. In individuals with diabetes, the body either does not produce enough insulin or does not effectively use the insulin it produces, leading to elevated blood sugar levels.
Diabetic shots involve the injection of insulin to supplement or replace the body’s natural insulin production. By delivering insulin directly into the bloodstream, diabetic shots help control blood sugar levels, preventing both hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar). This regulated blood sugar management is crucial for preventing long-term complications associated with diabetes, such as heart disease, stroke, kidney disease, and nerve damage.
The type of insulin used in diabetic shots, as well as the dosage and injection frequency, is tailored to individual needs and may change over time. Regular monitoring of blood sugar levels is essential to ensure effective diabetic shot therapy and to adjust the treatment plan as needed.
In summary, insulin is the key component of diabetic shots, enabling the effective absorption of glucose into cells. Diabetic shots provide a means to regulate blood sugar levels, preventing complications and improving the overall health and well-being of individuals with diabetes.
Subcutaneous
Subcutaneous injection is the primary method of administering diabetic shots, delivering insulin or other glucose-lowering medications just beneath the skin’s surface. This method is preferred for diabetic shots due to its simplicity, effectiveness, and relatively low risk of complications.
The subcutaneous tissue, located between the skin and muscle layers, provides an ideal site for insulin injection. It allows for easy and convenient injection using small needles, minimizing discomfort and maximizing patient acceptance. Additionally, the subcutaneous tissue ensures gradual absorption of insulin into the bloodstream, providing a more sustained effect compared to other injection methods.
The subcutaneous injection technique involves pinching a fold of skin and injecting the medication into the raised area. This technique helps prevent inadvertent injection into muscle or blood vessels, reducing the risk of pain, bleeding, or nerve damage. Proper injection technique and regular site rotation are essential to minimize skin irritation and ensure effective insulin absorption.
In summary, the subcutaneous method of injection is a crucial component of diabetic shots, offering a safe, convenient, and effective means of insulin delivery. Understanding the principles of subcutaneous injection empowers individuals with diabetes to self-manage their condition effectively, leading to improved blood sugar control and overall well-being.
Blood sugar control
Diabetic shots are primarily aimed at regulating blood sugar levels, a critical aspect of diabetes management. Elevated blood sugar levels, if left uncontrolled, can lead to a cascade of complications, including damage to blood vessels, nerves, and organs. Diabetic shots help individuals achieve and maintain optimal blood sugar levels, reducing the risk of these complications.
The effectiveness of diabetic shots in controlling blood sugar is well-established. Studies have shown that insulin therapy, the cornerstone of diabetic shots, significantly reduces HbA1c levels, a measure of long-term blood sugar control. By maintaining blood sugar within a healthy range, diabetic shots prevent the onset and progression of diabetic complications, such as heart disease, stroke, kidney disease, and retinopathy.
In summary, diabetic shots play a vital role in blood sugar control, providing a means to manage diabetes effectively and prevent the associated complications. The ability of diabetic shots to regulate blood sugar levels makes them an essential component of diabetes management, improving the overall health and well-being of individuals with this condition.
Complication prevention
Diabetic shots are not merely a means of managing blood sugar levels; they play a pivotal role in preventing the onset and progression of severe, long-term complications associated with diabetes. Elevated blood sugar levels, if left unchecked, can wreak havoc on the body’s blood vessels, nerves, and organs, leading to a range of debilitating conditions.
Diabetic shots, by effectively regulating blood sugar, mitigate the risk of these complications. For instance, uncontrolled blood sugar levels can damage the delicate blood vessels in the eyes, kidneys, and heart, leading to retinopathy, nephropathy, and cardiovascular disease, respectively. Diabetic shots help prevent or delay the development of these complications by maintaining blood sugar within a healthy range.
The connection between diabetic shots and complication prevention is of paramount importance. Diabetic shots empower individuals with diabetes to take an active role in safeguarding their long-term health. By adhering to prescribed diabetic shot regimens and maintaining optimal blood sugar levels, they can significantly reduce the likelihood of developing the debilitating complications associated with diabetes.
Medication options
Diabetic shots encompass a range of medication options, including various types of insulin and other glucose-lowering medications. These options are meticulously tailored to meet the unique needs of each individual with diabetes, ensuring optimal blood sugar control and management.
-
Rapid-acting insulin:
This type of insulin takes effect quickly, within 15-30 minutes of injection, and lasts for a shorter duration, typically 3-5 hours. It is often used before meals to counter the post-meal rise in blood sugar levels.
-
Short-acting insulin:
Short-acting insulin begins working within 30-60 minutes of injection and lasts for around 5-8 hours. It is commonly used before meals or snacks to manage blood sugar levels around mealtimes.
-
Intermediate-acting insulin:
Intermediate-acting insulin has a gradual onset of action, taking effect within 1-2 hours of injection, and lasts for 12-18 hours. It is often used once or twice a day to provide a steady background level of insulin.
-
Long-acting insulin:
Long-acting insulin has a slow and prolonged onset of action, taking effect several hours after injection, and can last for up to 24 hours or more. It is typically used once a day to provide a consistent level of insulin throughout the day.
The choice of insulin type and dosage for diabetic shots is highly individualized and depends on factors such as the type of diabetes, blood sugar levels, lifestyle, and individual response to insulin. Regular monitoring of blood sugar levels and close collaboration with a healthcare professional are crucial to determine the most effective medication regimen for each person.
Technological advancements
Technological advancements have revolutionized diabetic shot therapy, enhancing its precision and convenience, and empowering individuals with diabetes to manage their condition more effectively. Key innovations include insulin pumps and continuous glucose monitors (CGMs).
-
Insulin pumps:
Insulin pumps are small, computerized devices that deliver insulin continuously throughout the day, mimicking the body’s natural insulin production. They offer precise insulin delivery, allowing for adjustments based on blood sugar levels, mealtimes, and activity levels. Insulin pumps can significantly improve blood sugar control and reduce the risk of hypoglycemia and hyperglycemia.
-
Continuous glucose monitors (CGMs):
CGMs are small, wearable devices that continuously monitor glucose levels in the interstitial fluid. They provide real-time data on blood sugar trends, fluctuations, and patterns. CGMs allow individuals to make informed decisions about insulin dosing, diet, and activity, and can help prevent dangerous blood sugar excursions.
The integration of insulin pumps and CGMs has led to the development of advanced hybrid closed-loop systems, also known as artificial pancreases. These systems combine the continuous insulin delivery of an insulin pump with the real-time glucose monitoring of a CGM, automating insulin delivery based on blood sugar levels. Hybrid closed-loop systems further enhance blood sugar control, reduce the burden of diabetes management, and improve the quality of life for individuals with diabetes.
Technological advancements in diabetic shot therapy continue to evolve, with the promise of even more precise, convenient, and effective ways to manage diabetes. These innovations empower individuals with diabetes to take an active role in their care, leading to improved health outcomes and a better quality of life.
Diabetic Shot FAQs
The following are frequently asked questions about diabetic shots, providing concise and informative answers to common concerns and misconceptions.
Question 1: What is a diabetic shot?
A diabetic shot is an injection of insulin or other glucose-lowering medication to manage blood sugar levels in individuals with diabetes. Insulin is a hormone that helps glucose enter cells for energy.
Question 2: How often do I need to take diabetic shots?
The frequency of diabetic shots varies depending on the type of insulin, blood sugar levels, and individual needs. It is essential to follow the prescribed dosing schedule provided by a healthcare professional.
Question 3: Where do I inject diabetic shots?
Diabetic shots are typically injected subcutaneously, just beneath the skin, in areas such as the abdomen, thighs, or buttocks. Proper injection technique and site rotation are important to prevent skin irritation.
Question 4: Can I take diabetic shots with other medications?
It is important to inform a healthcare professional about all medications being taken, as some may interact with diabetic shots. Combining medications should be done under the guidance of a healthcare professional to ensure safety and effectiveness.
Question 5: Are there any side effects of diabetic shots?
Common side effects of diabetic shots include skin irritation at the injection site, weight gain, and hypoglycemia (low blood sugar). It is important to monitor blood sugar levels regularly and report any unusual symptoms to a healthcare professional.
Question 6: How can I minimize the pain of diabetic shots?
Using thin needles, injecting at room temperature, and rotating injection sites can help minimize pain. Applying a cold compress or massaging the injection area can also help reduce discomfort.
These FAQs provide a brief overview of diabetic shots. It is important to consult with a healthcare professional for personalized advice and guidance on diabetic shot therapy and diabetes management.
Transition to the next article section: Understanding the Importance of Blood Sugar Control in Diabetes
Tips for Effective Diabetic Shot Therapy
Diabetic shots play a crucial role in managing blood sugar levels and preventing complications in individuals with diabetes. Here are some essential tips to enhance the effectiveness of diabetic shot therapy:
Tip 1: Proper Injection Technique
Ensure correct injection technique to optimize insulin absorption and minimize discomfort. Inject subcutaneously, at a 90-degree angle, into clean skin. Rotate injection sites regularly to prevent lipohypertrophy (fatty lumps).
Tip 2: Accurate Dosing and Timing
Adhere to the prescribed insulin dosage and injection schedule. Consistent timing of shots helps maintain stable blood sugar levels. Monitor blood sugar levels regularly to adjust insulin doses as needed.
Tip 3: Meal Planning and Physical Activity
Coordinate diabetic shots with mealtimes and physical activity. Insulin requirements may vary depending on carbohydrate intake and exercise intensity. Plan meals and activities accordingly to prevent blood sugar spikes or drops.
Tip 4: Storage and Handling
Store insulin properly according to the manufacturer’s instructions. Avoid exposing insulin to extreme temperatures or sunlight. Use clean needles and syringes to prevent infection and ensure accurate dosing.
Tip 5: Travel Considerations
When traveling, pack insulin and supplies carefully. Inform security personnel about the need for diabetic supplies and medications. Adjust insulin doses if necessary to account for time zone changes.
Tip 6: Emergency Preparedness
Carry glucagon for emergency treatment of severe hypoglycemia. Educate family, friends, or colleagues on the signs and treatment of hypoglycemia and hyperglycemia.
Following these tips can significantly improve the effectiveness and safety of diabetic shot therapy. By adhering to proper injection techniques, maintaining accurate dosing, and considering meal planning and physical activity, individuals with diabetes can optimize blood sugar control and minimize the risk of complications.
Transition to the article’s conclusion: The Importance of Medication Adherence in Diabetes Management
Conclusion
Diabetic shots have revolutionized the management of diabetes, enabling individuals to effectively regulate their blood sugar levels and prevent complications. Through the advancement of insulin therapy, subcutaneous injection techniques, and technological innovations, diabetic shots have become an integral part of diabetes care.
The effective use of diabetic shots requires proper injection technique, accurate dosing, meal planning, and physical activity considerations. Adherence to these principles, along with proper storage, handling, and emergency preparedness, optimizes the benefits of diabetic shot therapy. By following these guidelines, individuals with diabetes can harness the power of diabetic shots to achieve optimal blood sugar control and improve their overall health and well-being.
Youtube Video: