Diabetes tipo 2 is a chronic condition where the body is unable to produce enough insulin, or does not use insulin well. This leads to high blood sugar levels, which can cause long-term damage to the heart, blood vessels, eyes, kidneys, and nerves.
Diabetes tipo 2 is the most common form of diabetes, affecting around 90% of people with the condition. It is often associated with obesity, physical inactivity, and family history, but it can also occur in people who are not overweight.
Symptoms of Diabetes Tipo 2 can include increased thirst, frequent urination, unexplained weight loss, increased hunger, and fatigue. Treatment for Diabetes Tipo 2 usually involves lifestyle changes, such as eating a healthy diet, getting regular exercise, and losing weight. If these measures are not enough to control blood sugar levels, medication may be prescribed.
Diabetes tipo 2 is a serious condition, but it can be managed with proper treatment. By following a healthy lifestyle and taking medication as prescribed, people with diabetes tipo 2 can live long, healthy lives.
Diabetes Tipo 2
Diabetes tipo 2 is a chronic condition that affects the body’s ability to produce or use insulin, leading to high blood sugar levels. Understanding the key aspects of diabetes tipo 2 is crucial for effective management and prevention.
- Chronic condition: Diabetes tipo 2 is a lifelong condition that requires ongoing management.
- Insulin resistance: The body’s cells become less responsive to insulin, leading to high blood sugar levels.
- Blood sugar control: Managing blood sugar levels is essential to prevent complications.
- Lifestyle factors: Obesity, physical inactivity, and unhealthy diet contribute to the development of diabetes tipo 2.
- Genetic predisposition: Family history increases the risk of developing diabetes tipo 2.
- Complications: Uncontrolled diabetes can lead to heart disease, stroke, kidney failure, and blindness.
- Management: Treatment involves lifestyle changes, medication, and regular monitoring.
In summary, diabetes tipo 2 is a complex condition that requires a comprehensive approach to management. By understanding the key aspects discussed above, individuals can take proactive steps to prevent or manage diabetes tipo 2, reducing the risk of complications and improving their overall health and well-being.
Chronic condition
Diabetes tipo 2 is a chronic condition that affects the body’s ability to produce or use insulin, leading to high blood sugar levels. This chronic condition requires ongoing management to prevent complications and maintain overall health and well-being.
- Lifestyle modifications: Managing diabetes tipo 2 involves adopting lifestyle modifications, such as maintaining a healthy diet, engaging in regular physical activity, and achieving and maintaining a healthy weight. These modifications help improve insulin sensitivity and control blood sugar levels.
- Medication: In some cases, medication may be necessary to manage diabetes tipo 2. Medications can help lower blood sugar levels and improve insulin sensitivity. Insulin therapy may also be required in some individuals.
- Regular monitoring: Regular monitoring of blood sugar levels is crucial for managing diabetes tipo 2. This allows individuals to track their blood sugar levels and make necessary adjustments to their management plan, such as adjusting medication or lifestyle factors.
- Complications prevention: Ongoing management of diabetes tipo 2 is essential to prevent complications. Uncontrolled diabetes can lead to severe health problems, including heart disease, stroke, kidney failure, and blindness. Proper management helps reduce the risk of developing these complications and promotes overall health.
In summary, the chronic nature of diabetes tipo 2 necessitates ongoing management to maintain blood sugar levels within a healthy range and prevent complications. This involves a combination of lifestyle modifications, medication, regular monitoring, and a commitment to maintaining a healthy lifestyle.
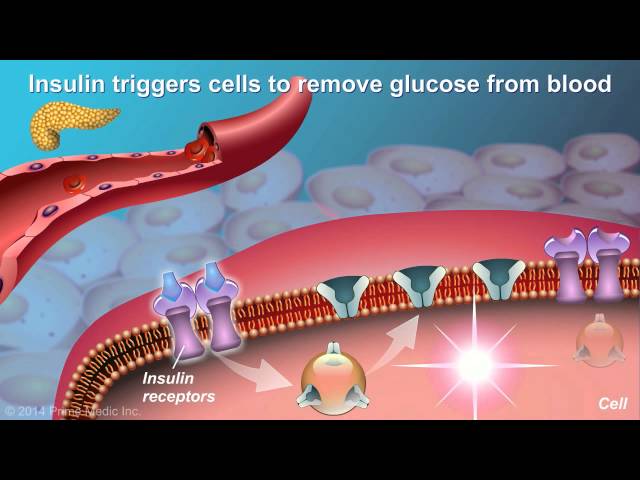
Insulin resistance
Insulin resistance is a condition in which the body’s cells do not respond properly to insulin, a hormone that helps glucose enter cells for energy. As a result, glucose builds up in the bloodstream, leading to high blood sugar levels.
Insulin resistance is a major factor in the development of type 2 diabetes. When cells become insulin resistant, the pancreas produces more insulin to overcome the resistance. Over time, the pancreas may not be able to produce enough insulin to keep blood sugar levels under control.
There are a number of factors that can contribute to insulin resistance, including obesity, physical inactivity, and a diet high in processed foods and sugary drinks. Insulin resistance can also be caused by certain medical conditions, such as Cushing’s syndrome and polycystic ovary syndrome.
Insulin resistance is a serious condition that can lead to a number of health problems, including type 2 diabetes, heart disease, stroke, and kidney disease. There is no cure for insulin resistance, but it can be managed with lifestyle changes, such as losing weight, eating a healthy diet, and getting regular exercise.
Blood sugar control
In the context of diabetes tipo 2, managing blood sugar levels is of paramount importance in preventing complications. Uncontrolled blood sugar levels can lead to severe health issues, including heart disease, stroke, kidney failure, and blindness.
- Preventing long-term damage: Sustained high blood sugar levels can damage blood vessels and nerves, leading to complications such as heart disease and kidney failure.
- Reducing the risk of blindness: Uncontrolled blood sugar levels can damage the blood vessels in the retina, potentially leading to blindness.
- Lowering the risk of amputation: High blood sugar levels can damage nerves and blood vessels in the feet, increasing the risk of foot ulcers and amputation.
- Improving overall health and well-being: Managing blood sugar levels can alleviate symptoms such as fatigue, excessive thirst, and frequent urination, leading to improved overall health and well-being.
Therefore, individuals with diabetes tipo 2 must prioritize blood sugar control through lifestyle modifications, medication, and regular monitoring. By doing so, they can significantly reduce the risk of developing severe complications and maintain a better quality of life.
Lifestyle factors
Lifestyle factors play a significant role in the development of diabetes tipo 2, which is characterized by insulin resistance and elevated blood sugar levels. Obesity, physical inactivity, and unhealthy diet are key contributors to the onset and progression of this condition.
- Obesity: Excess body weight, particularly abdominal obesity, is strongly linked to the development of diabetes tipo 2. Adipose tissue releases hormones and inflammatory factors that contribute to insulin resistance and impaired glucose metabolism.
- Physical inactivity: Regular physical activity improves insulin sensitivity and glucose utilization. Conversely, a sedentary lifestyle decreases insulin sensitivity and increases the risk of diabetes tipo 2.
- Unhealthy diet: A diet high in processed foods, sugary drinks, and unhealthy fats can contribute to weight gain and insulin resistance. These foods often have a high glycemic index, leading to rapid spikes in blood sugar levels and increased insulin demand.
The interaction between these lifestyle factors can create a vicious cycle, where obesity leads to physical inactivity and an unhealthy diet, further exacerbating insulin resistance and the progression of diabetes tipo 2. Addressing these lifestyle factors through healthy eating, regular exercise, and weight management is crucial for the prevention and management of diabetes tipo 2.
Genetic predisposition
Genetic predisposition plays a significant role in the development of diabetes tipo 2. Family history is a strong indicator of an individual’s risk of developing the condition, as genetic factors account for approximately 20-25% of cases.
People with a family history of diabetes tipo 2 have inherited certain genetic variations that make them more likely to develop the condition. These genetic variations can affect the body’s ability to produce or use insulin, leading to insulin resistance and elevated blood sugar levels.
While genetic predisposition increases the risk of developing diabetes tipo 2, it does not guarantee that an individual will develop the condition. Environmental factors, such as obesity, physical inactivity, and unhealthy diet, also play a significant role in the onset and progression of the disease.
Understanding the connection between genetic predisposition and diabetes tipo 2 is crucial for individuals with a family history of the condition. By being aware of their increased risk, they can take proactive steps to reduce their chances of developing the disease. This may involve adopting a healthy lifestyle, including regular exercise, a balanced diet, and maintaining a healthy weight.
In conclusion, genetic predisposition is a significant risk factor for diabetes tipo 2. Individuals with a family history of the condition should be aware of their increased risk and take steps to mitigate it through lifestyle modifications. Early detection and prevention strategies are essential for managing diabetes tipo 2 and preventing its complications.
Complications
Uncontrolled diabetes tipo 2 can lead to several severe complications, including heart disease, stroke, kidney failure, and blindness. These complications arise from the chronic elevation of blood sugar levels, which damages blood vessels and organs over time.
- Cardiovascular complications: High blood sugar levels can damage the blood vessels that supply blood to the heart, leading to the development of heart disease. This can manifest as chest pain, shortness of breath, and an increased risk of heart attack and stroke.
- Kidney damage: Diabetes tipo 2 can also damage the kidneys, which are responsible for filtering waste products from the blood. Over time, uncontrolled blood sugar levels can lead to kidney failure, requiring dialysis or a kidney transplant.
- Retinopathy: Diabetes tipo 2 can damage the blood vessels in the retina, leading to a condition called retinopathy. This can cause blurred vision, vision loss, and even blindness if left untreated.
- Neuropathy: High blood sugar levels can also damage the nerves, leading to a condition called neuropathy. This can cause numbness, tingling, and pain in the hands, feet, and legs.
These complications highlight the importance of managing blood sugar levels in diabetes tipo 2. By maintaining healthy blood sugar levels, individuals can significantly reduce their risk of developing these severe complications and preserve their overall health and well-being.
Management
Managing diabetes tipo 2 involves a multifaceted approach that includes lifestyle changes, medication, and regular monitoring. These components are interconnected and play a crucial role in maintaining blood sugar levels within a healthy range and preventing complications.
Lifestyle changes, such as adopting a balanced diet, engaging in regular physical activity, and achieving a healthy weight, can significantly improve insulin sensitivity and glucose metabolism. By making these changes, individuals with diabetes tipo 2 can reduce their reliance on medication and improve their overall health and well-being.
Medication may be necessary when lifestyle changes alone are not sufficient to control blood sugar levels. Medications for diabetes tipo 2 work by increasing insulin production, enhancing insulin sensitivity, or reducing the absorption of glucose from the digestive tract. Regular monitoring of blood sugar levels is essential to assess the effectiveness of treatment and make necessary adjustments.
The connection between management and diabetes tipo 2 is evident in the improved health outcomes associated with effective management. By adhering to treatment plans, individuals with diabetes tipo 2 can reduce their risk of developing severe complications, such as heart disease, stroke, kidney failure, and blindness.
In summary, the management of diabetes tipo 2 through lifestyle changes, medication, and regular monitoring is crucial for maintaining blood sugar control and preventing complications. Understanding this connection empowers individuals to take an active role in managing their condition and improving their quality of life.
FAQs about Diabetes Tipo 2
This section provides answers to commonly asked questions about diabetes tipo 2, empowering individuals to better understand and manage their condition.
Question 1: What is diabetes tipo 2?
Diabetes tipo 2 is a chronic condition characterized by the body’s inability to produce or effectively use insulin, leading to elevated blood sugar levels.
Question 2: What are the symptoms of diabetes tipo 2?
Common symptoms include increased thirst, frequent urination, unexplained weight loss, fatigue, and blurred vision.
Question 3: What causes diabetes tipo 2?
Risk factors include family history, obesity, physical inactivity, and unhealthy diet.
Question 4: How is diabetes tipo 2 treated?
Treatment involves lifestyle modifications, such as adopting a healthy diet and engaging in regular exercise, as well as medication to manage blood sugar levels.
Question 5: Can diabetes tipo 2 be prevented?
While not always preventable, maintaining a healthy weight, engaging in regular physical activity, and following a balanced diet can reduce the risk of developing diabetes tipo 2.
Question 6: How can I manage diabetes tipo 2 effectively?
Effective management requires regular blood sugar monitoring, adherence to medication regimens, and ongoing lifestyle modifications to maintain healthy blood sugar levels and prevent complications.
Understanding these key aspects of diabetes tipo 2 empowers individuals to take an active role in managing their condition, improving their quality of life, and reducing the risk of severe complications.
Transition to the next article section: For further insights and comprehensive information on diabetes tipo 2, explore the following resources…
Tips for Managing Diabetes Tipo 2
Managing diabetes tipo 2 effectively requires a comprehensive approach that includes lifestyle modifications, medication, and regular monitoring. Here are some practical tips to help you manage your condition and improve your overall health:
Tip 1: Follow a Healthy Diet
- Choose whole, unprocessed foods over processed or packaged foods.
- Increase your intake of fruits, vegetables, and whole grains.
- Limit your intake of sugary drinks, processed carbohydrates, and unhealthy fats.
Tip 2: Engage in Regular Physical Activity
- Aim for at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous-intensity exercise per week.
- Choose activities that you enjoy and can fit into your schedule.
- Regular exercise helps improve insulin sensitivity and blood sugar control.
Tip 3: Maintain a Healthy Weight
- Excess weight can contribute to insulin resistance and worsen diabetes management.
- Set realistic weight loss goals and make gradual changes to your lifestyle.
- Losing even a small amount of weight can have significant benefits.
Tip 4: Take Medications as Prescribed
- If your doctor prescribes medication, take it exactly as directed.
- Do not skip or adjust your medication without consulting your doctor.
- Medication can help lower blood sugar levels and improve insulin sensitivity.
Tip 5: Monitor Your Blood Sugar Levels Regularly
- Regular blood sugar monitoring is essential for managing diabetes effectively.
- Follow your doctor’s instructions on how and when to check your blood sugar levels.
- Keep a record of your readings to track your progress and make necessary adjustments.
These tips provide a foundation for managing diabetes tipo 2. By following these recommendations, you can improve your blood sugar control, reduce your risk of complications, and live a healthier, more fulfilling life.
Remember: Managing diabetes is a journey, not a destination. There will be challenges along the way, but with dedication and support, you can achieve your health goals.
Diabetes Tipo 2
Diabetes tipo 2 is a chronic condition that requires ongoing management, but it can be successfully managed with a combination of lifestyle modifications, medication, and regular monitoring. Understanding the key aspects of diabetes tipo 2, such as insulin resistance, blood sugar control, and the importance of managing risk factors, is crucial for effective management and prevention.
By adopting a healthy lifestyle, taking medication as prescribed, and monitoring blood sugar levels regularly, individuals with diabetes tipo 2 can significantly reduce their risk of developing severe complications and maintain a good quality of life. Remember, managing diabetes is a journey that requires dedication and support, but with the right approach, it is a journey towards better health and well-being.
Youtube Video: