Diabetic shots refer to injections of insulin, a hormone naturally produced by the pancreas that regulates blood sugar levels. Individuals with diabetes may require insulin therapy to manage their condition due to the body’s inability to produce enough insulin or use it effectively.
Insulin injections are crucial for maintaining blood sugar control, preventing complications such as nerve damage, eye problems, and kidney disease. Historically, insulin was extracted from animal pancreases, but advancements in biotechnology have led to the production of synthetic human insulin, offering greater purity and consistency.
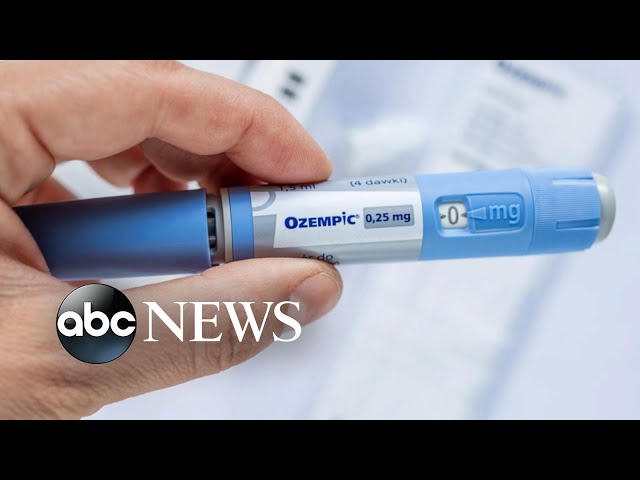
Diabetic shots can be administered using various devices, including syringes, pens, and insulin pumps. Healthcare professionals provide personalized guidance on injection techniques, dosage, and timing to optimize blood sugar management. Regular monitoring of blood sugar levels is essential to adjust insulin doses as needed and prevent both high and low blood sugar episodes.
diabetic shots
Diabetic shots, referring to insulin injections, play a crucial role in diabetes management. Key aspects related to diabetic shots include:
- Administration: Injections via syringes, pens, or pumps.
- Dosage: Personalized based on individual needs and blood sugar levels.
- Timing: Injections taken as per prescribed schedules.
- Insulin types: Rapid-acting, short-acting, intermediate-acting, and long-acting insulin.
- Blood glucose monitoring: Essential for adjusting insulin doses.
- Complications: Potential risks include hypoglycemia (low blood sugar) and lipohypertrophy (fatty lumps at injection sites).
- Education and support: Healthcare professionals provide guidance and support for effective insulin therapy.
Diabetic shots are essential for individuals with diabetes to maintain blood sugar control and prevent complications. Proper administration, monitoring, and ongoing education are crucial for successful insulin therapy. Regular communication with healthcare providers is vital to optimize insulin regimens and achieve good glycemic control.
Administration
Administration of diabetic shots involves injecting insulin into the body using various devices, namely syringes, pens, or pumps. Each method has its own advantages and considerations.
- Syringes: Traditionally used for insulin injections, syringes offer precise dosage control and are cost-effective. However, multiple daily injections may be required, and syringe use requires proper technique to avoid discomfort or complications.
- Pens: Insulin pens are pre-filled devices that resemble large pens. They are convenient and discreet, making them suitable for injections on the go. Pens offer ease of use, reducing the risk of dosing errors.
- Pumps: Insulin pumps provide continuous subcutaneous insulin delivery through a small, wearable device. Pumps offer precise control over insulin administration, allowing for customized basal rates and bolus doses. They are particularly beneficial for individuals with highly variable blood sugar levels or those seeking improved glycemic control.
The choice of administration method depends on individual preferences, lifestyle, and medical needs. Healthcare providers can guide patients in selecting the most appropriate device and provide training on proper injection techniques.
Dosage
The dosage of diabetic shots is not a one-size-fits-all approach. It is personalized based on individual needs and blood sugar levels. Several factors influence insulin dosage, including body weight, activity level, diet, and blood sugar control goals.
Determining the appropriate insulin dosage requires regular monitoring of blood sugar levels. This can be done using a blood glucose meter, which measures the amount of glucose in a small drop of blood. Based on the blood sugar readings, healthcare providers make adjustments to the insulin dosage to achieve optimal glycemic control.
The importance of personalized insulin dosage cannot be overstated. Too little insulin can lead to high blood sugar levels, increasing the risk of complications such as diabetic ketoacidosis. Conversely, too much insulin can cause hypoglycemia, a condition characterized by dangerously low blood sugar levels.
Regular monitoring of blood sugar levels and close collaboration with healthcare providers are crucial for determining and adjusting insulin dosage. This personalized approach to diabetic shots empowers individuals with diabetes to manage their condition effectively and prevent complications.
Timing
In the context of diabetic shots, timing plays a crucial role in achieving effective blood sugar control. Insulin injections must be taken as per prescribed schedules to ensure optimal insulin activity and prevent blood sugar fluctuations.
-
Maintaining Stable Blood Sugar Levels:
Regularly scheduled insulin injections help maintain stable blood sugar levels throughout the day. This prevents extreme highs and lows in blood sugar, reducing the risk of both hyperglycemia and hypoglycemia. -
Matching Insulin Action to Mealtimes:
Timing insulin injections around meals allows insulin to be present when blood sugar levels rise after eating. This helps prevent post-meal blood sugar spikes and improves overall glycemic control. -
Preventing Dawn Phenomenon:
The dawn phenomenon is a natural rise in blood sugar levels that occurs in the early morning hours. Taking insulin before bedtime can help counteract this phenomenon and prevent high blood sugar levels upon waking. -
Reducing Injection Frequency:
Long-acting insulin formulations can be taken once or twice a day, reducing the frequency of injections and improving convenience for patients.
Adhering to prescribed injection schedules is essential for effective diabetes management. By taking insulin shots at the right time, individuals can optimize blood sugar control, prevent complications, and improve their overall well-being.
Insulin types
In the context of diabetic shots, the type of insulin used is crucial for achieving optimal blood sugar control. Several types of insulin are available, each with its unique characteristics and duration of action:
- Rapid-acting insulin: Onset within 15 minutes; lasts for 3-4 hours; used to cover meals.
- Short-acting insulin: Onset within 30 minutes; lasts for 6-8 hours; also used to cover meals.
- Intermediate-acting insulin: Onset within 2-4 hours; lasts for 12-18 hours; used to provide basal coverage.
- Long-acting insulin: Onset within 4-6 hours; lasts for 24 hours or more; used to provide basal coverage.
The choice of insulin type depends on individual needs and preferences. Some people may require a combination of different insulin types to achieve optimal glycemic control. Healthcare providers work with patients to determine the most appropriate insulin regimen based on factors such as lifestyle, blood sugar patterns, and overall health status.
Understanding the different types of insulin and their duration of action is essential for effective diabetes management. By selecting the right insulin type and injection schedule, individuals with diabetes can optimize blood sugar control, prevent complications, and improve their quality of life.
Blood glucose monitoring
Blood glucose monitoring is a crucial component of diabetic shots as it provides essential information for adjusting insulin doses to achieve optimal blood sugar control. Without regular blood glucose monitoring, individuals with diabetes would be unable to determine the effectiveness of their insulin therapy and make necessary adjustments to prevent blood sugar levels from becoming too high or too low.
Real-life examples illustrate the practical significance of blood glucose monitoring in diabetic shots. For instance, if an individual’s blood sugar levels are consistently high, it may indicate that their insulin dose is too low and needs to be increased. Conversely, if blood sugar levels are frequently dropping too low, it may suggest that the insulin dose is too high and needs to be reduced.
Understanding the connection between blood glucose monitoring and diabetic shots empowers individuals with diabetes to take an active role in managing their condition. By regularly checking their blood sugar levels and working closely with their healthcare providers, they can make informed decisions about their insulin doses and achieve better glycemic control.
Complications
Complications associated with diabetic shots primarily stem from two potential risks: hypoglycemia and lipohypertrophy. Hypoglycemia, or low blood sugar, occurs when insulin levels are too high relative to blood glucose levels. This can lead to symptoms such as shakiness, sweating, confusion, and in severe cases, seizures or loss of consciousness. Lipohypertrophy, on the other hand, refers to the formation of fatty lumps at injection sites. It results from repeated insulin injections in the same location, causing fat cells to enlarge and accumulate.
Understanding these complications is crucial for individuals using diabetic shots. Hypoglycemia can be dangerous and requires immediate treatment to raise blood sugar levels. Recognizing the symptoms of hypoglycemia and knowing how to respond appropriately is essential for preventing severe consequences.
Lipohypertrophy, while not as dangerous as hypoglycemia, can be bothersome and affect insulin absorption. Rotating injection sites and using proper injection techniques can help prevent lipohypertrophy.
Regular monitoring of blood sugar levels and proper injection practices are key to minimizing the risks associated with diabetic shots. Individuals using insulin should work closely with their healthcare providers to develop a personalized treatment plan that optimizes blood sugar control while minimizing the likelihood of complications.
Education and support
In the context of diabetic shots, education and support play a vital role in empowering individuals to manage their condition effectively. Healthcare professionals, including doctors, nurses, diabetes educators, and pharmacists, provide comprehensive guidance and support to ensure successful insulin therapy.
-
Understanding Insulin Therapy:
Healthcare professionals educate individuals about the different types of insulin, their mechanisms of action, and how to adjust doses based on blood sugar levels. They also provide training on proper injection techniques to ensure safe and effective insulin administration. -
Monitoring Blood Sugar:
Regular blood sugar monitoring is crucial for managing diabetes. Healthcare professionals guide individuals on how to use blood glucose meters, interpret results, and make informed decisions about insulin doses. They also emphasize the importance of keeping a log of blood sugar readings to track patterns and identify trends. -
Lifestyle Management:
Diabetes management extends beyond insulin therapy. Healthcare professionals provide guidance on healthy eating habits, regular exercise, and stress management techniques. They collaborate with individuals to develop personalized lifestyle plans that support overall well-being and glycemic control. -
Problem-Solving and Troubleshooting:
Inevitably, individuals using diabetic shots may encounter challenges or setbacks. Healthcare professionals serve as a valuable resource for problem-solving and troubleshooting. They provide support and guidance on managing hypoglycemia, preventing lipohypertrophy, and addressing other potential complications.
The education and support provided by healthcare professionals are fundamental to the success of diabetic shots. By empowering individuals with knowledge, skills, and ongoing support, healthcare professionals enable them to take an active role in their diabetes management, optimize insulin therapy, and achieve better health outcomes.
Frequently Asked Questions about Diabetic Shots
Diabetic shots, also known as insulin injections, play a crucial role in managing diabetes. They provide the body with the insulin it needs to regulate blood sugar levels. Here are answers to some frequently asked questions about diabetic shots:
Question 1: What types of insulin are available for injection?
There are several types of insulin available, including rapid-acting, short-acting, intermediate-acting, and long-acting insulin. Each type has a different onset and duration of action. Healthcare professionals will recommend the most appropriate type or combination of types based on individual needs.
Question 2: How often should I inject insulin?
The frequency of insulin injections varies depending on the type of insulin used and individual needs. Some people may need to inject insulin multiple times a day, while others may only need to inject once or twice a day.
Question 3: What are the potential side effects of insulin injections?
Potential side effects of insulin injections include hypoglycemia (low blood sugar), lipohypertrophy (fatty lumps at injection sites), and allergic reactions. However, these side effects can be minimized by using proper injection techniques and working closely with a healthcare professional to manage insulin therapy.
Question 4: Can I take oral medications instead of insulin injections?
In some cases, oral medications may be an option for managing diabetes. However, insulin injections are often necessary for people with type 1 diabetes or those who do not respond well to oral medications.
Question 5: How can I learn to inject insulin properly?
Healthcare professionals can provide training on proper injection techniques. They will teach individuals how to choose the right injection site, insert the needle correctly, and administer the insulin safely.
Question 6: What should I do if I miss an insulin injection?
If an insulin injection is missed, it is important to take it as soon as possible. However, if it is close to the time for the next injection, it may be best to skip the missed dose and take the next one as scheduled. It is crucial to consult with a healthcare professional for guidance in such situations.
Summary: Diabetic shots are an essential part of diabetes management for many individuals. Understanding the different types of insulin, injection techniques, and potential side effects is crucial for successful insulin therapy. Regular monitoring of blood sugar levels and close collaboration with healthcare professionals are vital for optimizing insulin doses and achieving good glycemic control.
Transition to the next article section: For more information on diabetic shots and diabetes management, please refer to the following resources:
Diabetic Shot Tips
Diabetic shots, also known as insulin injections, are a crucial part of managing diabetes. Here are some tips for administering diabetic shots safely and effectively:
Tip 1: Choose the Right Injection Site:
Rotate injection sites to prevent lipohypertrophy (fatty lumps) and ensure proper insulin absorption. Common injection sites include the abdomen, thighs, buttocks, and upper arms.
Tip 2: Use Proper Injection Technique:
Insert the needle straight into the skin at a 90-degree angle. Inject the insulin slowly and steadily, and hold the needle in place for 5-10 seconds afterward.
Tip 3: Store Insulin Properly:
Unopened insulin should be refrigerated at 36-46F (2-8C). Once opened, it can be stored at room temperature for up to 28 days. Avoid freezing insulin.
Tip 4: Monitor Blood Sugar Regularly:
Regular blood sugar monitoring is crucial for adjusting insulin doses and preventing hypoglycemia (low blood sugar). Use a blood glucose meter to check blood sugar levels as directed by your healthcare professional.
Tip 5: Travel with Insulin:
When traveling, carry insulin in a cool bag with an ice pack. Inform airport security about your insulin and supplies. Keep a medical ID card with you in case of emergencies.
Tip 6: Avoid Alcohol Before Injections:
Alcohol can interfere with insulin absorption. Avoid drinking alcohol for at least 1 hour before and after insulin injections.
Following these tips can help individuals using diabetic shots optimize insulin therapy, minimize risks, and improve their overall diabetes management.
Remember, proper diabetic shot administration is essential for effective blood sugar control. Consult with your healthcare professional for personalized guidance and support.
Conclusion
Diabetic shots, or insulin injections, play a crucial role in managing diabetes. They provide the body with the insulin it needs to regulate blood sugar levels, preventing complications and improving overall health. Understanding the different types of insulin, proper injection techniques, and potential side effects is paramount for successful insulin therapy.
Regular monitoring of blood sugar levels and close collaboration with healthcare professionals are vital for optimizing insulin doses and achieving good glycemic control. By adhering to recommended guidelines and seeking professional support, individuals using diabetic shots can effectively manage their diabetes, improve their quality of life, and reduce the risk of long-term complications.
Youtube Video: